A multidisciplinary team from China has successfully transplanted a gene-modified pig liver into a human recipient diagnosed with brain death. During a 10-day observation period, the porcine liver produced bile and porcine albumin, maintained stable blood flow, and showed no signs of rejection.
The report of the transplantation — published in the journal Nature — is the first known peer-reviewed publication describing the transplantation of a gene-modified pig liver to a human, according to a press statement.
This is an “important experiment,” as it opens up the possibility of using a porcine liver as a “temporary replacement of the diseased liver until a human liver can be obtained for the definitive transplant,” said Rafael Matesanz, MD, PhD, creator and founder of the National Transplant Organization in Spain, in a roundup from the Science Media Centre (SMC).
Performing xenotransplants in patients with brain death but hemodynamic stability is a “frequent approach,” before moving on to the clinical phase, “so that the evolution of the organ and the impact on the deceased person’s organism can be assessed at least in the short term,” explained Matesanz, who was not involved in the procedure.
The group from China has conducted liver xenotransplantation research for more than a decade. In 2013, they successfully performed the first pig-to-monkey heterotopic auxiliary liver transplantation in China. Both the recipient monkey and the transplanted liver survived for 14 days.
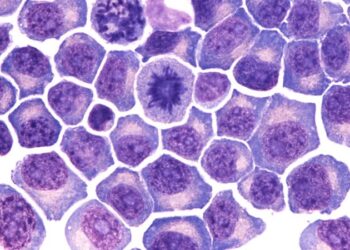
In the current case, the donor liver came from a pig that had been genetically modified to inactivate genes that mediate rejection and to include human transgenes to facilitate compatibility.
Before transplant, Ke-Feng Dou, Xijing Hospital, Fourth Military Medical University, Xi’an, China, and colleagues used flow cytometry to confirm the success of these modifications. They then transplanted the liver from the pig to the brain-dead recipient.
They used “a very elegant surgical technique, which allows the insertion of a (relatively small) xeno-liver with limited disruption to the anatomy of the existing liver,” commented Peter Friend, MD, FRCS, professor of transplantation at the University of Oxford, Oxford, England, in the SMC roundup.
After transplantation, the Chinese team monitored graft function, blood flow, and immune and inflammatory responses over a 10-day period.
Immune responses were controlled with immunosuppressants. “T-cell activity was inhibited by antithymocyte globulin administration, and B-cell activation increased 3 days after surgery and was then inhibited by rituximab. There were no significant perioperative changes in immunoglobulin G or immunoglobulin M levels. C-reactive protein and procalcitonin levels were initially elevated and then quickly declined,” the study team reported.
Alanine aminotransferase levels remained in the normal range, while aspartate aminotransferase levels increased on postoperative day 1 and then rapidly declined.
These preliminary findings suggest that gene-modified pig livers can survive and function in humans, potentially serving as a bridge therapy for patients with liver failure, the investigators said. However, they noted that the length of the study was limited.
“At the request of the recipient’s family members, the study was terminated on day 10, which made the follow-up period insufficient to analyze alterations in xenograft function over a long period,” they explained.
Additionally, the team could only measure basic liver functions, such as the synthesis of albumin and the secretion of bile. Further research is needed to evaluate long-term outcomes and the full range of liver functions, they said.
“I found the work very relevant, but we have to be cautious,” Iván Fernández Vega, professor of pathological anatomy at the University of Oviedo, Oviedo, Spain, told the SMC.
“Although this is a pioneering advance, studies with a larger sample and in living recipients will be necessary to confirm the safety, efficacy, and reproducibility of the procedure.”
Xenotransplantation is an active area of clinical research. As reported previously by Medscape Medical News, research teams in the United States have performed pig-to-human heart transplantation and pig-to-human kidney transplantation.
Source link : https://www.medscape.com/viewarticle/first-gene-modified-pig-liver-transplanted-human-2025a10007gp?src=rss
Author :
Publish date : 2025-03-28 11:00:00
Copyright for syndicated content belongs to the linked Source.