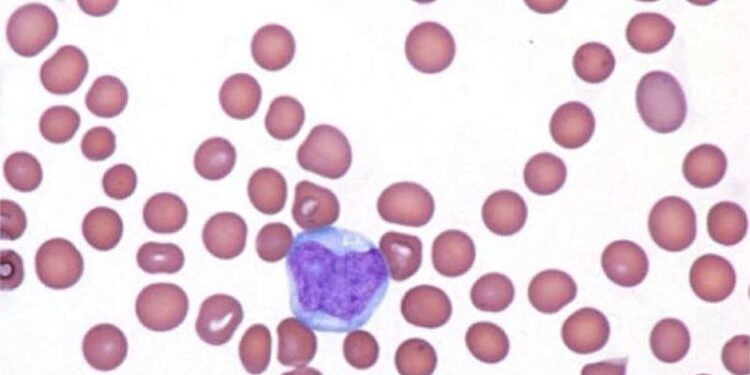
CHICAGO — The antibody-drug conjugate (ADC) pivekimab sunirine (PVEK) yielded high response rates with good durability in patients with blastic plasmacytoid dendritic cell neoplasm (BPDCN) in the phase 1/2 CADENZA trial.
“We conclude that PVEK represents a potentially practice-changing paradigm for patients with the rare disease BPDCN,” said study author Naveen Pemmaraju, MD, of MD Anderson Cancer Center in Houston, Texas, during an oral abstract session at the American Society of Clinical Oncology (ASCO) 2025 annual meeting. “One half of first-line patients treated with PVEK subsequently received stem cell transplant. PVEK treatment had a manageable safety profile, and infusion-related reactions and peripheral edema were resolved with supportive care. No capillary-leak syndrome was observed.”
CADENZA enrolled 84 adult patients with CD123-positive BPDCN. Of these patients, 33 were newly diagnosed, and 51 patients had relapsed or refractory (R/R) BPDCN with one, two, or three prior lines of therapy. In the first-line group, 22 patients had de novo disease and 11 had a prior or concomitant hematologic malignancy (PCHM).
CADENZA’s primary endpoint was the composite rate of complete response (CR) plus CR with minimal skin abnormality (CRc) in the first-line de novo patients.
The authors found that 70% of patients achieved the composite CR, while 14% of the patients with R/R disease did. Regarding the overall response rate (ORR), 85% of first-line patients responded to PVEK, while 35% of patients with R/R disease responded.
Responses among patients with R/R disease were early and durable (median, 1.4 months and 9.2 months, respectively).
PCHM status did not affect overall survival (OS) in first-line patients: Median OS was 16.6 months in both the de novo and PCHM subgroups.
The discussant for this study, Raajit Rampal, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York City, told Medscape Medical News that the CADENZA trial supports the use of CD123 as a therapeutic target in BPDCN. He also noted that the current standard of care often causes potentially life-threatening capillary leak syndrome (CLS): “There were no cases of CLS in this dataset, which means we may have an opportunity to deliver anti-CD123 therapies, with no CLS as a potential side effect.”
Rampal also cited PVEK’s apparent ability to enable many patients to bridge to stem cell transplant, “the fundamental prospect in terms of long-term survival provisions with BPDCN.”
Following this presentation, Pemmaraju sat down with Medscape Medical News. The following interview has been edited for clarity.
Please give us some context on BPDCN and why it is difficult to treat.
BPDCN is a rare, aggressive hematologic malignancy primarily involving skin, bone marrow, lymph nodes and the central nervous system. We think there are only 500 BPDCN diagnoses per year in the United States. Current treatment regimens are limited to chemotherapy regimens adapted from AML, ALL, lymphoma, and myeloma. The median age at diagnosis is around 65 years, so many patients are not eligible for intensive chemo or stem cell transplant. CD123 is overexpressed on all BPDCN blasts, making it an ideal target for immunochemotherapy.
What is the top takeaway from your presentation?
BPDCN has an overall poor prognosis with significant unmet need. Currently, tagraxofusp-erzs is the standard of care and the only approved treatment for BPDCN. PVEK is a new CD123-targeting agent. This novel monotherapy, given once every 3 weeks, had high response rates for frontline patients with BPDCN and was highly durable. Even for patients with R/R disease, whose prognosis is only a few months, PVEK showed some promising activity both in response and durability.
Patients with BPDCN are in need of improved frontline therapies to treat their disease, so we’re very excited to see this phase 1/2 trial going extremely well in terms of safety and efficacy. The responses we have observed make PVEK a strong candidate as a standard-of-care treatment.
What is another important thing you want your colleagues to know about this study?
The CADENZA trial enrolled 84 patients, which is a huge number in a rare disease field like ours. I’m proud we were able to achieve a real-world demographic split. That means we had older patients, just like I see in the clinic, and half the patients had skin involvement along with bone marrow. In the relapsed group, the prior therapy had been quite intense. Half of these patients had received chemo, half had received tagraxofusp, and a third had received a transplant. This may be the best study I’ve ever done in terms of enrolling patients who are truly representative with all the comorbidities, and all the difficulties, you see in clinical practice.
You mentioned that PVEK is more patient-friendly than the standard of care. Why is that?
PVEK is given once every 3 weeks via an infusion that takes only 30 minutes or less. Many of our other drugs, of course, require a much more intensive schedule that can be difficult for patients, especially when they must be given on an inpatient basis. PVEK can be given outpatient even from the beginning, which is much more convenient for patients.
You referred several times to patients’ skin lesions. Is that part of the BPDCN disease process or is that a treatment reaction?
I want to emphasize this is a BPDCN trait not related to treatment. BPDCN has a predilection for the skin. The vast majority of patients with BPDCN, anywhere from 70% to 90%, will present with skin findings. It’s very common for my patients to present with “just” a skin lesion that turns out to be anything but. Unlike other skin-containing malignancies, BPDCN is a bone marrow blood cancer that can go to an acute leukemia and become acutely life threatening. Let’s differentiate that from the cutaneous toxicity very commonly seen in chemo-based regimens.
What’s ahead in PVEK research?
We will keep presenting our data, including at the European Hematological Association and as an ASCO Encore presentation. We hope to submit PVEK to regulatory agencies in the near future. Ultimately, can we combine PVEK with other agents active in the AML and BPDCN space to create a next-generation therapy? Eventually, once we have two active agents for BPDCN, we will need to determine the sequencing of these drugs. What’s the natural history of these treated patients? Are they living longer? I think answers to all those questions will come out in the coming year or two.
The study was funded by AbbVie.
Pemmaraju disclosed having relationships with AbbVie, Aplastic Anemia and MDS International Foundation, Aptitude Health, Astellas Pharma, Blueprint Medicines, Bristol Myers Squibb, CancerNet, CareDx, Celgene, Cimeio Therapeutics, ClearView Healthcare Partners, CTI BioPharma Corp, Curio Science, Dava Oncology, EUSA Pharma, Harborside Press, Imedex, ImmunoGen, Intellisphere, Magdalen Medical Publishing, Medscape, Menarini Group, Neopharm, Novartis, OncLive, Pacylex, Patient Power, Peerview, PharmaEssentia, and Physicians’ Education Resource.
Rampal reported having ties with AbbVie, Blueprint Medicines, Bristol Myers Squibb/Celgene, Constellation Pharmaceuticals, CTI BioPharma Corp, Disc Medicine, Galecto, Incyte, Karyopharm Therapeutics, Novartis, Pharmaessentia, Promedior, SERVIER, Sierra Oncology, Stemline Therapeutics, Sumitomo Dainippon, and Zentalis.
Darcy Lewis writes about clinical medicine from Chicago.
Source link : https://www.medscape.com/viewarticle/pvek-new-standard-care-rare-deadly-blood-cancer-2025a1000f77?src=rss
Author :
Publish date : 2025-06-05 12:09:00
Copyright for syndicated content belongs to the linked Source.