TOPLINE:
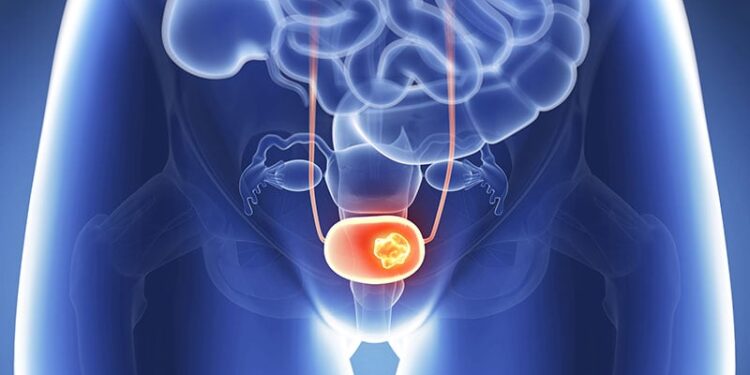
In patients with muscle-invasive bladder cancer, trimodal therapy modestly improved quality of life compared with radical cystectomy but was not cost-effective at either 5 or 10 years. The high costs associated with trimodal therapy exceeded commonly accepted “willingness-to-pay” thresholds, a new analysis found.
METHODOLOGY:
- Trimodal therapy, which includes maximal transurethral resection followed by chemotherapy and radiation, is an alternative for patients who are unable or unwilling to undergo radical cystectomy. However, there are no randomized trials comparing the two approaches, and data on cost and utility trade-offs are limited.
- Researchers compared the cost-effectiveness of trimodal therapy and radical cystectomy using a simulation model that incorporates health economics. The index patient reflected patients in a large 2023 retrospective study: aged 71 years with clinical stage T2-4aN0M0 muscle-invasive bladder cancer, solitary tumor < 7 cm in size, adequate bladder function, and no multifocal or extensive carcinoma in situ.
- The model simulated outcomes over 5 and 10 years, using cost data from a Medicare payer perspective (adjusted to 2021 US dollars) and assumed the two treatment approach es had equivalent oncologic efficacy.
- Primary outcomes included costs, effectiveness measured in quality-adjusted life years (QALYs), and incremental cost-effectiveness ratios (ICERs). Cost-effectiveness was assessed using a willingness-to-pay threshold of $100,000 per QALY.
TAKEAWAY:
- The average cost of trimodal therapy was more than $30,000 higher than the cost of radical cystectomy at 5 years ($71,014 vs $40,489) and 10 years ($85,137 vs $49,570).
- Trimodal therapy demonstrated a small advantage over radical cystectomy in terms of quality of life, due to fewer acute and long-term toxic effects: 3.94 vs 3.87 QALYs at 5 years and 6.61 vs 6.49 QALYs at 10 years.
- Compared to radical cystectomy, trimodal therapy was not cost-effective overall at either timepoint, with ICERs of $464,291 per QALY at 5 years and $308,636 per QALY at 10 years. However, trimodal therapy was considered cost-effective for 21% of patients at 10 years — supporting its use for some “appropriately counseled” patients.
- Sensitivity analysis revealed that trimodal therapy would become broadly cost-effective if the initial cost dropped by more than half (to $17,605), or if it achieved an 11.6% improvement in metastasis-free survival.
IN PRACTICE:
The results underscore two ongoing needs: a better understanding of patients’ long-term outcomes with trimodal therapy vs radical cystectomy and measures to rein in the high cost of bladder cancer care. “These findings highlight the importance of developing policy initiatives that help reduce [trimodal therapy] costs and of providing patients with accurate expectations of long-term toxic effects to help guide preference-sensitive care,” the study authors wrote.
SOURCE:
The study, led by Daniel Joyce, MD, MS, Vanderbilt University Medical Center, Nashville, Tennessee, was published online in JAMA Network Open.
LIMITATIONS:
The findings were limited by model assumptions and potential selection bias from the retrospective studies used. The model inputs were based on the best available evidence. All nonmuscle-invasive recurrences after trimodal therapy were assumed to be treated with Bacillus Calmette-Guérin, possibly overestimating costs by excluding intravesical chemotherapy options.
DISCLOSURES:
The authors did not disclose any funding information. Several authors declared receiving consulting fees or grants or having other ties with various sources.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Source link : https://www.medscape.com/viewarticle/trimodal-therapy-costs-offset-qol-benefit-muscle-invasive-2025a1000h4b?src=rss
Author :
Publish date : 2025-06-26 04:15:00
Copyright for syndicated content belongs to the linked Source.