Individuals living with both HIV and hepatitis C virus (HCV) who ultimately developed hepatocellular carcinoma (HCC) showed greater suppression of plasma extracellular vesicles (pEVs) after HCV clearance than those who did not develop cancer, based on new data presented at the International AIDS Society Conference on HIV Science.
The study is important because of the persistent risk for HCC among individuals with advanced fibrosis who clear HCV with direct-acting antivirals, said Ariel Osegueda, MSc, a PhD candidate and biologist at the University of Buenos Aires, Buenos Aires, Argentina, in an interview.
pEVs are essential in immune modulation. Natural killer (NK) cells are essential for immune surveillance, particularly in targeting tumor cells, and CD107a (also known as lysosomal-associated membrane protein-1) is an indicator of cytotoxic activity.
“Understanding how natural killer cell function is modulated in this context may reveal mechanisms linked to that increased risk,” said Osegueda, who presented the findings at the meeting.
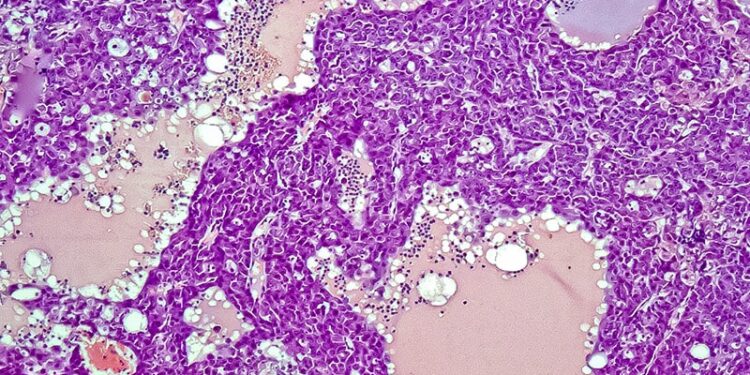
The researchers collected plasma samples from 11 adults with advanced liver disease at baseline and after treatment with direct-acting antivirals. A total of five patients developed HCC after a median of 5.75 years after clearance. The researchers also assessed samples from six healthy control individuals. NK cell degranulation was assessed using flow cytometry.
The pEV from individuals with advanced LF at baseline were significantly more suppressive than control individuals (0.71 vs 0.88; P = .023). By at least 1 year after direct-acting antiviral therapy, pEV in patients who developed HCC was significantly more suppressive than in those who did not develop HCC (0.75 vs 0.86; P = .008). In addition, the pEV among individuals who did not develop HCC was similar to control individuals, whereas pEV from those who ultimately developed HCC was more suppressive than control individuals (P = .03).
Overall, the presence of pEV from all study participants, including control individuals, reduced expression of NK CD107a expression compared to NK cells without pEV. NK suppression persisted over time in patients who developed HCC but decreased in those who did not.
The researchers were particularly surprised by the persistent NK suppression seen in patients who developed HCC, Osegueda told Medscape Medical News. “This suggests an early and lasting immune alteration not reversed by viral clearance,” she said.
This study was limited by the small sample size, but there are implications for clinical practice, Osegueda said. “Persistent NK dysfunction mediated by plasma extracellular vesicles could become a biomarker to identify patients at higher risk of hepatocellular carcinoma after HCV cure,” she said.
However, larger studies are needed to confirm these findings, characterize the pEV content, and explore whether modulating NK function can reduce HCC risk, Osegueda added.
Foundation for Future Studies
“The risk of HCC remains elevated for patients living with HIV who have liver fibrosis despite HCV cure,” said David J. Cennimo, MD, associate professor of medicine and pediatrics in the Division of Infectious Disease at Rutgers New Jersey Medical School, Newark, New Jersey, in an interview.
In the current study, the researchers present early data that could help identify a risk factor for liver cancer, said Cennimo, who was not involved in the study. The study also sheds light on the impact of the immune system’s surveillance in preventing cancer by closer examination of pEVs, he said.
This study was funded by a grant from the National Agency for Research, Technological Development and Innovation (Argentina).
The authors had no financial disclosures.
Cennimo had no financial disclosures.
Source link : https://www.medscape.com/viewarticle/new-biomarker-may-predict-advancement-hcc-hiv-hcv-2025a1000kcw?src=rss
Author :
Publish date : 2025-07-31 11:58:00
Copyright for syndicated content belongs to the linked Source.