[ad_1]
A minimally invasive surgical procedure for glaucoma designed to reduce intraocular pressure (IOP) has been found to have a high degree of success and significantly reduce the use of drugs for the condition.
The procedure, ab interno canaloplasty, is a form of minimally invasive glaucoma surgery performed from inside the eye rather than through an external incision. The technique involves the use of an iTrack or iTrack Advance microcatheter to open channels at the front of the eye to enable drainage of fluid.
An analysis of 465 eyes in a global data registry that had undergone ab interno canaloplasty for primary and secondary open-angle glaucoma with showed a 70% success rate and lowered IOP by at least 20% in half the patients. The study defined postoperative success as a reduction in IOP of 20% or more or a reduction to below 18 mm Hg with either no change or a reduction in glaucoma medications.
“This study demonstrates that ab interno canaloplasty using the iTrack or iTrack Advance is effective in lowering IOP and reducing medication dependence across various glaucoma types and severities, with a favorable safety profile up to 36 months postoperatively,” Shamil Patel, MD, a glaucoma specialist at Eye Physicians & Surgeons of Arizona, told Medscape Medical News. Patel presented the findings at the 2025 meeting of the American Glaucoma Society. The results are in line with what other studies found with ab interno canaloplasty, he added.
The Canaloplasty Procedure
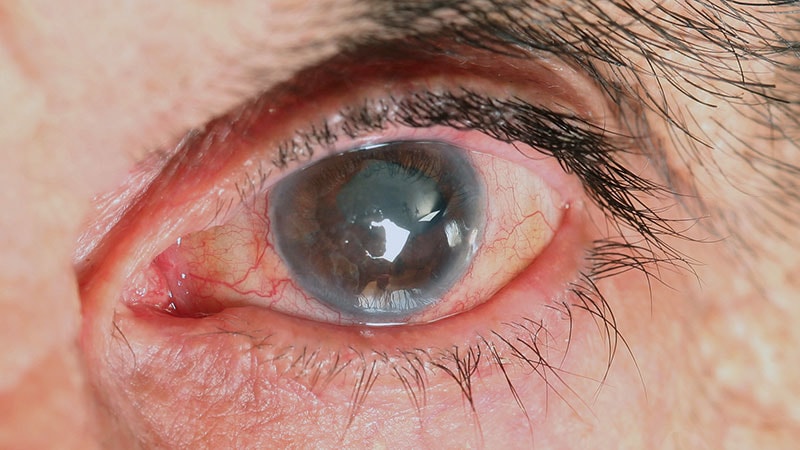
Canaloplasty is a surgical procedure for glaucoma that targets main structures that channel the outflow of aqueous fluid at the front of the eye, such as the trabecular meshwork, Schlemm’s canal, and the distal collector channels. Uninterrupted drainage of aqueous fluid allows the eye to maintain normal pressure, but when those channels are blocked, it can cause pressure to increase, which is a biomarker of glaucoma.
The ab interno procedure Patel’s study evaluated involves inserting a flexible microcatheter 360 degrees around the Schlemm’s canal to clear blockages, then injecting viscoelastic fluid into the Schlemm’s canal as the microcatheter is withdrawn. This process dilates the Schlemm’s canal and improves the function of the trabecular meshwork to allow aqueous fluid drainage.
Viscoelastic agents are gel-like solutions injected in the front of the eye during surgery to maintain a space in which to operate while protecting ocular structures. The agents are removed after the operation.
The iTrack is indicated for fluid infusion or aspiration during surgery, whereas iTrack Advance is indicated for catheterization and viscodilation of Schlemm’s canal to reduce IOP in adults with open-angle glaucoma.
Study Results
Upon enrollment in the study, the average IOP was 18.1 mm Hg (± 6.10), and patients were on an average of two medications (± 1.18). At 12 months, the average IOP was 13.8 mm Hg per eye (± 4.03), and patients were taking fewer than one drug on average (P < .001). At 24 months, those numbers were 12.7 mm Hg (± 3.09) and 1.26 (± 1.43) (n = 43, P < .001), respectively.
In 89.9% of cases, canaloplasty was performed concurrently with cataract surgery, while the remainder of the eyes had canaloplasty only. On enrollment in the study, 8.7% of eyes did not need antiglaucoma medication; at 24 months post-canaloplasty, 51.2% of eyes were medication-free.
“The procedure had a strong safety profile, with no sight-threatening complications and a low rate [1.9%] of additional glaucoma surgery,” Patel said. The overall complication rate was 2.5%, he reported.
The prospective, multicenter design of the study; its real-world nature; and standardized collection of data were strengths of research, Patel said. Potential limitations were the lack of a control group, no randomization, and a large pool of patients who were lost to follow-up, as well as IOP measures at enrollment while patients were still taking their glaucoma medications.
“Despite these limitations, the study provides robust real-world evidence supporting the safety and effectiveness of ab interno canaloplasty with iTrack,” Patel said.
Zachary Vest, MD, a glaucoma specialist in Sheridan, Colorado, said the size of the study was noteworthy. “In a lot of glaucoma studies, having more than 400 eyes is quite impressive,” Vest said. “From a safety standpoint having 250 in an efficacy population, that’s a quite healthy number.”
The study also provided evidence on the safety of the use of a microcatheter in canaloplasty, Vest added. One of the concerns with using a microcatheter during canaloplasty has been the volume of viscoelastic the operation requires, he said.
“This really shows it is unusual for there to be significant post-op issues directly related to canaloplasty,” Vest said. One of the major potential complications with the surgery is detachment of the Descemet’s membrane, a thin, elastic layer within the cornea.
“They only had one with this technique, and that’s always been one of those things that’s been a specter around this technique from its early external canaloplasty days,” he said. “That’s a great benefit.”
Patel is a consultant to Nova Eye Medical. Vest disclosed financial relationships with Glaukos, Alcon, and Elios Vision.
Richard Mark Kirkner is a medical journalist based in Philadelphia.
[ad_2]
Source link : https://www.medscape.com/viewarticle/real-world-study-minimally-invasive-canaloplasty-glaucoma-2025a10006h0?src=rss
Author :
Publish date : 2025-03-18 12:59:00
Copyright for syndicated content belongs to the linked Source.