US regulators’ use of a speedy clearance pathway for a new frontline indication for asciminib for chronic myeloid leukemia (CML) has raised questions due to the number of medications already available for this condition.
In October, the US Food and Drug Administration (FDA) granted accelerated approval to asciminib (Scemblix, Novartis AG) for adult patients with newly diagnosed Philadelphia chromosome–positive CML in chronic phase.
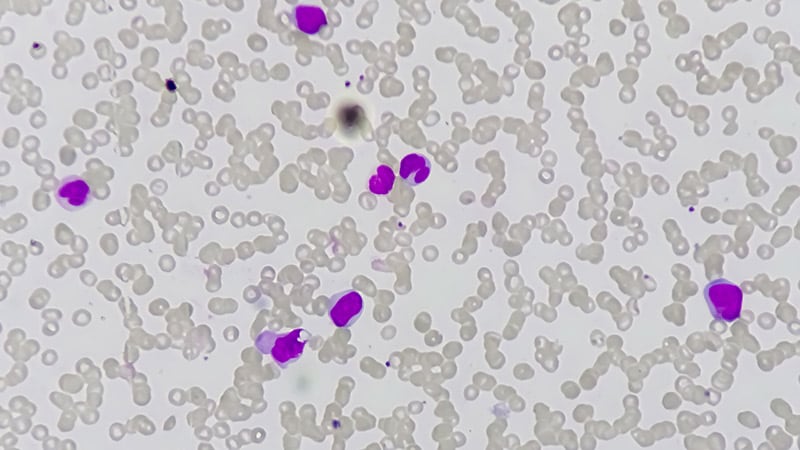
Asciminib is one of the six tyrosine kinase inhibitor (TKI) drugs used for CML, a class that began with the introduction of imatinib (Gleevec) in 2001. By 2016, researchers reported that TKIs had helped make life expectancy in patients with CML approach that of the general population. Physicians and patients now have several options of second-generation TKI drugs that also can be used in newly diagnosed patients, along with the option to begin with the more affordable option of imatinib.
The FDA in 1992 instituted the accelerated approval pathway to try to speed market drugs for serious conditions that fill unmet medical needs.
The agency and companies essentially make bets on promising study results, often using surrogate markers, to allow sales of medicines while waiting for evidence from confirmatory studies. For example, the FDA in August used the accelerated approval process to clear the first T-cell receptor gene therapy for certain advanced forms of sarcoma, a form of cancer with limited treatment options.
The next accelerated approval of a cancer drug was the indication for asciminib as a frontline therapy. The FDA also used accelerated approval for the initial clearance of asciminib in 2021 for use in CML previously treated with two or more TKIs. By 2022, Novartis presented sufficient evidence of the drug’s merit to win full approval for the drug in this use.
The timeline is longer for the expected confirmatory research for asciminib as a frontline therapy, with a 2028 deadline set for this work. The data presented to date on asciminib have not persuaded some oncologists on the need for the speedy approval of frontline use.
“This boils down to a drug that looks as if it’s just as good as other second-generation TKIs,” Mikkael A. Sekeres, MD, MS, chief of the Division of Hematology at the Sylvester Comprehensive Cancer Center, University of Miami Health System, Miami. “I don’t know how they could use the accelerated approval mechanism to get this through.”
Sekeres, a former chair of the Oncologic Drugs Advisory Committee, explored concerns and challenges involved with the use of the accelerated approval process in his 2022 book, Drugs and the FDA: Safety, Efficacy, and the Public’s Trust.
“The intent of the accelerated approval mechanism is that you’re bringing a new therapy to treat a serious disease in a way that others haven’t previously, where there aren’t existing options,” Sekeres said.
This is a markedly different situation that exists for CML, where medicines have improved dramatically in the 21st century, unlike many other forms of cancer treated by hematologists.
“As someone who specializes in treating people with leukemia, I’d be happy every clinic day of my life if all of my patients came in with chronic phase, chronic myeloid leukemia,” instead of other cancers lacking these robust treatment options, he said.
With CML, physicians select among TKIs considering side effects and other health conditions patients have, including weighing the impact of financial toxicity in some cases, he said.
“If I have a patient with lower risk chronic phase, chronic myeloid leukemia, I’m treating them with imatinib,” Sekeres said.
Questions About Surrogate Endpoints
Sekeres is not alone in questioning the use of the speedier FDA pathway for a new indication for a TKI in CML.
“Where is the ‘unmet need’ justifying an accelerated approval in this setting?” wrote Timothée Olivier, MD, who is affiliated with both the Hôpitaux universitaires de Genève and the VK Prasad Laboratory funded by Vinay Prasad, MD, MPH, in a November 3 post on X.
Olivier, Prasad, and coauthors in a September correspondence to the American Journal of Hematology raised questions about the study design for a key asciminib study, ASC4FIRST. They noted what they consider a weakness with the endpoints used.
“Molecular milestones like the 48-week MMR [measles, mumps, and rubella vaccination] are often used in clinical trials due to their convenience and shorter timeline for assessment,” they wrote. “However, these milestones are not definitive indicators of long-term survival or overall clinical benefit.”
There has been rising concern in recent years about the evidence gap between initial accelerated approvals and the completion of studies that show whether these promising therapies actually help patients live longer or better. Researchers including Bishal Gyawali, MD, PhD, a Medscape Medical News contributor, also have questioned the degree of reliance on surrogate endpoints in accelerated approvals.
In response, the FDA’s Cancer Division and the US Congress have taken steps to try to force drugmakers to more quickly answer the key question in accelerated approvals: Does this medicine produce the expected benefits? For example, the FDA in March appears to have turned down a bid for accelerated approval of a lymphoma drug due to concerns about the timing of completion of confirmatory research.
The use of accelerated approval will continue to be a balancing act, due in part to demand for newer agents, said Ravi Bhatia, MD, of the O’Neal Comprehensive Cancer Center at The University of Alabama at Birmingham, in an email to Medscape Medical News.
“Accelerated approval of agents for up-front treatment of CML does not appear well justified, given the high degree of efficacy of existing agents,” said Bhatia, who is vice chair of the National Comprehensive Cancer Network’s Clinical Practice Guidelines in Oncology Panel for Chronic Myeloid Leukemia.
“On the other hand, there is greater urgency for developing agents for patients who have failed existing agents and patients with advanced phase disease, and the use of accelerated approval may be justified in this setting,” Bhatia said.
In an interview with Medscape Medical News, Richard A. Larson, MD, a professor in the Department of Hematology/Oncology at The University of Chicago, Chicago, who is an ASC4FIRST investigator, noted the 96-week follow-up data from the trial will be presented at the annual meeting of the American Society of Hematology in December in San Diego.
Larson said data from this trial will show continued benefit with the frontline use of asciminib. Larson also is an author of a New England Journal of Medicine article in May about the ASC4FIRST trial.
“The data speak for themselves, that asciminib is at least as effective or more so and at least as well tolerated as what’s already on the market,” Larson said. “So their argument, at the end of the day, really boils down to the cost of a new drug and whether we need a new drug.”
From the point of view of patients with cancer, the answer to that is clear, he said.
“If you talk to cancer patients, they’d like to see new drugs become available as quickly as possible. And I think that was the original rationale for the accelerated approval pathway, that a drug that has been shown to be safe and effective in a prospective clinical trial could get accelerated approval based on a surrogate endpoint.”
The remarkable success seen in developing TKI drugs for CML creates difficulties in testing later entrants in this class due to their prolonged survival, Larson said.
“If you look on a population basis, the overall survival of newly diagnosed CML patients with all of these therapeutic options available to them now approximate that of the non-CML population.”
“For most anticancer drugs, the FDA would like to see an overall survival benefit, but patients with newly diagnosed CML are surviving 20 or 30 years, and they’re not dying at an accelerated rate the way they were. So it’d be impractical to require a clinical trial to show a survival benefit, a randomized trial.”
“That’s where the use of a surrogate endpoint, which is the major molecular response at 1 year, has been so valuable, gets the drugs approved, gets them into patients far earlier than if there was a survival end point requirement,” he said.
Larson reported ties with AbbVie, Amgen, Astellas, Celgene, Cellectis, Curis, CVS Caremark, Daiichi Sankyo, ImmunoGen, Jazz, MorphoSys, Rigel, Servier, Forty Seven/Gilead, Novartis, and Rafael Pharmaceuticals. Sekeres disclosed relationships with BMS, Kurome, and Novartis Advisory Boards. Bhatia reported no relevant disclosures.
Kerry Dooley Young is a freelance journalist based in Washington, DC. Follow her on LinkedIn and Threads.
Source link : https://www.medscape.com/viewarticle/accelerated-approval-new-frontline-tki-use-cml-raises-2024a1000lx4?src=rss
Author :
Publish date : 2024-12-02 11:21:22
Copyright for syndicated content belongs to the linked Source.