Clinicians generally shouldn’t use potassium-competitive acid blockers (P-CAB) as first-line therapy for acid-related conditions, nonerosive gastroesophageal reflux disease (GERD), or peptic ulcer disease, according to a recent clinical practice update from the American Gastroenterological Association (AGA).
However, P-CABs are recommended in place of proton pump inhibitors (PPIs) for most patients with Helicobacter pylori and other conditions where patients haven’t responded to PPIs.
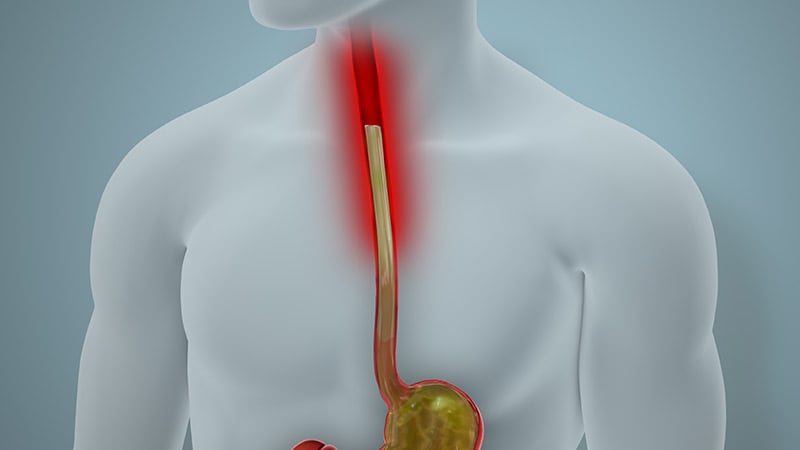
“P-CABs are a newer medication class now available in the US, associated with more rapid, potent, and prolonged gastric acid inhibition than PPI formulations,” said lead author Amit Patel, MD, a gastroenterologist at the Duke University School of Medicine and Durham Veterans Affairs Medical Center, Durham, North Carolina.
“P-CABs have potentially significant clinical benefits in the management of Helicobacter pylori infection and GERD, particularly more severe erosive esophagitis,” he said. “Emerging data are affording additional insights into the clinical benefits of P-CABs in settings such as on-demand therapy for reflux-associated symptoms, bleeding gastroduodenal ulcers, and endoscopic eradication therapy for Barrett’s esophagus.”
The update was published online in Gastroenterology.
P-CAB Developments
For most patients, PPIs and histamine-2 receptor antagonists remain the primary way to inhibit gastric acid secretion for common upper gastrointestinal conditions, the authors wrote. However, PCABs such as vonoprazan and tegoprazan may provide relief when PPIs have limitations.
Unlike PPIs, P-CABs are considered acid-stable, don’t require premeal dosing, aren’t prodrugs, and don’t require conversion to an active form to provide pharmacologic effects. They tend to have longer half-lives and more rapid onset. Serum gastrin levels typically remain higher with P-CABs.
In terms of safety, randomized trial data indicate that P-CABs are generally well tolerated and have short-term and medium-term safety similar to PPIs. Due to potent acid suppression, enteric infection risks remain higher, though long-term safety data is needed, the authors wrote.
Overall, P-CABs appear to be equally as potent or more potent than PPIs, though more potent acid inhibition isn’t necessarily associated with better outcomes, the authors wrote. For most foregut acid-related disorders — such as heartburn and prevention of nonsteroidal anti-inflammatory drug–associated ulcers — P-CABs can help when patients fail PPI therapy.
In general, though, nonclinical factors related to cost, barriers to obtaining medication, and limited long-term safety data may outweigh the advantages of P-CABs, especially if clinical superiority isn’t yet known, the authors wrote.
For GERD, clinicians generally shouldn’t use P-CABs as first-line therapy for patients with uninvestigated heartburn symptoms or nonerosive reflux disease. However, P-CABs should be used for those with documented acid-related reflux who fail therapy with twice-daily PPIs. They may also be appropriate for on-demand heartburn therapy, although more evidence is needed.
For erosive esophagitis, P-CABs generally shouldn’t be used for milder cases but can be considered for patients with more severe cases that haven’t responded to PPIs, including refractory esophagitis.
For H pylori, P-CABs should be used in place of PPIs for eradication regimens, including among patients with clarithromycin-resistant strains. In contrast with most of the other indications in the update, the short-term duration of H pylori treatment reduced the authors’ concerns about P-CAB costs and safety.
For peptic ulcer disease, P-CABs generally shouldn’t be used as first-line treatment or prophylaxis. However, the rapid onset and potent acid inhibition could be useful for patients with bleeding gastroduodenal ulcers and high-risk stigmata.
“Emerging data will allow refinements in the populations and clinical settings for which P-CABs at various doses may be considered and advised — and may reveal more clinical scenarios in which they can provide meaningful benefit,” Patel said. “Further investigations, including additional populations and novel indicators, as well as evaluating long-term safety data and cost-effectiveness, are warranted, as P-CABs are incorporated more broadly into clinical practice worldwide.”
P-CABs in Practice
For the first time in recent decades, P-CABs offer a new option to treat acid-related conditions and reflux disease, but clinicians remain confused about how to incorporate them into practice. Although the update is somewhat helpful, it still leaves unanswered questions, said Stuart Spechler, MD, chief of gastroenterology and co-director of the Center for Esophageal Diseases at Baylor University Medical Center, Houston, Texas.
“I was surprised that the update had a negative tone, which felt unwarranted in many cases,” he said. “Several of the best practice advice statements also seemed to be based on assumptions, especially regarding cost and availability, which I thought was odd for an update like this.”
Spechler expressed several concerns about the phrasing of the advice statements, particularly ones that lacked direct data, as well as nuances around PPI and P-CAB dosing, efficacy, and safety in clinical studies.
“My contention is that P-CABs offer a number of advantages and are probably better drugs in general, so as the physician who treats patients, I want to offer the best medicine for each patient,” he said. “Is that going to break the bank? With discounts available, I don’t think $25 per month is going to break the bank for most patients, and no doubt, the prices will continue to come down.”
Looking ahead, Spechler noted the value of additional studies focused on more nuanced efficacy, long-term safety, and cost-effectiveness data.
“Although P-CABs are new in this country, they’ve been used extensively in Japan for 10 years and appear to be as safe and effective as PPIs,” he said. “There’s a place for the use of these medications in clinical practice and practicing physicians should take this update under advisement as they consider how to best use them for their patients.”
The authors received no specific funding for this update. Patel and Spechler reported no relevant disclosures.
Carolyn Crist is a health and medical journalist who reports on the latest studies for Medscape Medical News, MDedge, and WebMD.
Source link : https://www.medscape.com/viewarticle/aga-clinical-practice-update-says-p-cabs-can-help-when-2025a10000jz?src=rss
Author :
Publish date : 2025-01-10 12:20:03
Copyright for syndicated content belongs to the linked Source.