These days, you can’t turn around without encountering some sort of artificial/augmented intelligence (AI). From generative AI invading your word processing to web searches, security systems, and manufacturing equipment, AI is ubiquitous. So it’s no surprise that AI is dominating the conversations in medicine, too. But as with every possible application of AI, along with the promise, there must be guardrails and caution.
That’s the stance from the American Medical Association (AMA), which had this to say on the matter: “The AMA believes it is critical that our country adopts a regulatory framework that ensures only safe, high-quality, unbiased, and clinically validated AI products are brought to market. For AI-enabled tools to truly live up to their promise, they must first earn — and then retain — the trust of patients and physicians. Just as we demand proof that new medicines and biologics are safe and effective, so must we insist on clinical evidence of the safety and efficacy of new AI-enabled healthcare applications.”
Despite the need for caution, a recent AMA physician survey revealed that doctors’ interest and enthusiasm in the technology is growing rapidly. Some 68% of respondents recognize AI’s benefits, up from 63% in 2023. Along with their feelings about the tools, AI use cases in practice is also on the rise. In 2023, 38% of respondents reported using AI, whereas in 2024, that number jumped to 62%. “The pressures on medicine right now are extraordinary,” said AMA immediate past president Jesse M. Ehrenfeld, MD. “We don’t have enough doctors or healthcare workers to meet the demands.”
The result is what the AMA survey shows — interest in AI is spiking. “The AI hype cycle is high, and that has opened up interest in every industry,” said Nishit Patel, MD, vice president and chief medical informatics officer at Tampa General Hospital, Tampa, Florida. “The medical industry is always looking at the evolution of technology to deliver better care and make clinicians more efficient.”
AI has arrived in medicine, that much is clear. But even with its promise, there are nuances and important considerations before a full, across-the-board buy in.
AI in Admin
One of the areas of medicine where AI offers promise is its ability to boost capacity in a field facing severe practitioner shortages.
“Healthcare is data heavy, and there’s tons of valuable information tucked away, which is an area where AI can prove valuable,” said Patel. “AI can generate content that takes the burden away from doctors sitting at their keyboards.”
At Tampa General, an ambient AI tool helps generate clinical documentation so that doctors can focus on the patient in front of them. “On average, for every hour a doctor spends with a patient, he or she spends two at the computer,” said Patel. “AI frees them up.”
From the AMA’s perspective, using AI in administrative tasks is a productive use of the technology. Tools like automated scribing technology can support documentation, which simplifies workflow and delivers time back to busy doctors. According to Ehrenfeld, this is an example of a low-stakes application — if AI makes a mistake (like a typo) or doesn’t produce a perfect transcription — it won’t affect a patient outcome.
At Tampa General, the team has built a data platform with medical records, and depending on the solution needed, will tap into different iterations of AI. This might include machine learning, which is algorithmic, rules-based AI that sets criteria, or generative AI language models.
In the clinical application space, the use of AI remains much lower, albeit growing. “We are acutely aware of the risks and errors associated with AI,” said Ehrenfeld. “There is a need to deal with that fact and manage AI’s use appropriately.”
For that reason, most hospitals and physicians are applying AI as a supplement — not a replacement — in the clinical setting.
AI in Patient Care
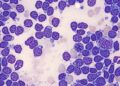
There is a wide array of patient care applications in the field of AI — pathology being one. Matthew Hanna, MD, a pathologist at Memorial Sloane Kettering Cancer Center, New York City, is integrating AI into his screening workflows. “The tools are designed to help pathologists identify two of the three markers on any given patient’s case,” he explained. “The goal is to support the patient safety net.”
Hanna shared the example of AI at work helping to diagnose tissue from an enlarged prostate. After a human team creates a biopsy of the prostate tissue, they digitize the slides, which creates pixels. Using an AI-assisted tool for prostate cancer detection, the machine learning model then screens from the digitized image and notifies doctors of its results. From there, the doctor reviews the report, comparing human findings to the tool’s findings. “It allows us to triage patients,” he said. “If it can save one patient’s life, especially in a rural area with overworked doctors, it’s worth it.”
All that said, Hanna is still cautious about AI and ensures a human writes the final report. “There’s no instance where AI is directly outputting to a patient chart,” he said. “But if AI is used in the diagnosis, there needs to be a disclaimer about that fact.”
Radiology is another space that is putting AI tools to work. This isn’t because they are perfect, emphasized Ehrenfeld, but because they can elevate a scan’s reading almost instantly. “This changes workflows that are otherwise challenging,” he said.
For example, in one hospital, a patient came in suffering from large blood clots on both sides of the body, along with an acute strain on his heart. A doctor ordered a CT scan, and in the background, AI read the exam instantly. In this case, the tool flagged the care team. The patient was in a life-threatening situation, and AI provided that information hours before a radiologist might have read the scan.
In this regard, Ehrenfeld said that the AMA prefers the approach of “augmented” intelligence, not artificial. “We want to emphasize the promise of the tools, but it’s important to say they will help humans, not replace them,” he said.
Likewise, there are hospital pharmacies using AI to determine the cost effectiveness of various treatments, and in some gerontology settings, clinicians are using the tool to identify cognitive decline to begin treatment earlier. At Tampa General, AI might “close a loop” when care teams see something concerning, according to Patel. “In the case of sepsis, when the condition gets out of control, the odds are 1 in 5 patients won’t leave the hospital,” he said. “This isn’t a diagnosis based on a single lab test, but a combination of tests, vitals, and other factors. AI can help put those pieces together and get patients onto antibiotics much faster.”
So much so, according to Patel, that his hospital has been able to lower its sepsis mortality rate to under 7% — the national average hovers around 15%-18%.
As AI continues to evolve, expect adoption rates to grow in medicine. “The industry is yearning for it,” said Ehrenfeld. “But we need a regulatory framework to ensure safe products are brought into the marketplace. Above all else, AI must be designed and deployed in an equitable, responsible, and transparent fashion.”
Source link : https://www.medscape.com/viewarticle/medicine-meets-ai-boom-promise-and-caution-go-hand-hand-2025a10006fa?src=rss
Author :
Publish date : 2025-03-18 08:29:00
Copyright for syndicated content belongs to the linked Source.