TOPLINE:
Analysis reveals initiating anal cancer screening at age 35 years or older among men who have sex with men (MSM) with HIV is cost-effective. A greater value was seen if screening was started at 35 years than at 40-45 years of age.
METHODOLOGY:
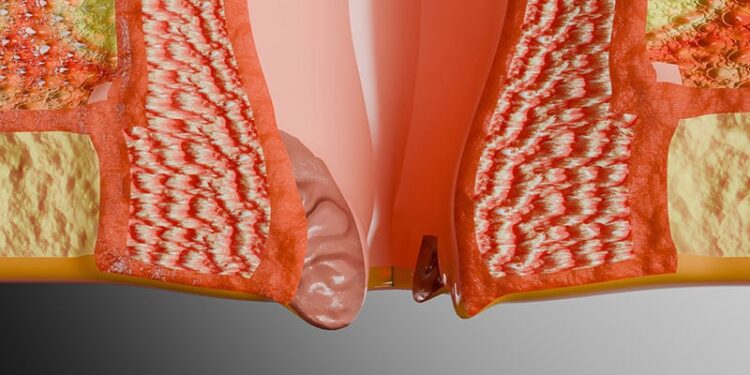
- MSM with HIV face a markedly elevated risk for anal cancer, with an incidence of 85 cases per 100,000 persons. The Anal Cancer-HSIL Outcomes Research (ANCHOR) trial recently demonstrated that anal high-grade squamous intraepithelial lesion (HSIL) treatment reduces anal cancer risk among people with HIV.
- A microsimulation model was developed to simulate the life course of MSM with HIV, including natural histories of HIV, human papillomavirus(HPV), HSIL, and anal cancer.
- Analysis included MSM with HIV aged 35 years or older in 2019 for the base-case analysis, with additional sensitivity analyses for newly eligible cohorts at 5-year increments up to age 55 years.
- Researchers evaluated cytology alone, HPV testing options, co-testing, and triage strategies across different screening intervals (annual, biennial, triennial, or quadrennial).
- Outcome measures encompassed incremental cost-effectiveness ratios in dollars per quality-adjusted life-year and tradeoff of harms vs benefits.
TAKEAWAY:
- Without screening, researchers predicted 4064 anal cancer cases and 680 deaths would occur over the lifetime of 100,000 MSM with HIV aged 35 years or older.
- Screening initiation at age 35 years demonstrated greater value than starting at age 40 or 45 years, with incremental cost-effectiveness ratio, $87,731 for quadrennial intervals to $350,100 for annual intervals.
- The quadrennial HPV16/18 strategy remained cost-effective through age 55 years, supporting screening initiation up to this age.
- Compared with no screening, anal cancer mortality reduction ranged from 25.8% for quadrennial cytology with HPV16 triage to 63.1% for annual cytology with high-risk HPV co-testing.
IN PRACTICE:
“Our model estimated that annual cytology screening among MSM with HIV aged 35 years or older could reduce anal cancer mortality by up to 65% and found that triennial cytology was cost-efficient vs screening at age 40 or 45 years or older and cost-effective vs no screening. In our comparative effectiveness analysis, HPV-based screening, particularly triennial testing for HPV16/18, was efficient,” the authors of the study wrote.
SOURCE:
This study was led by Ashish A. Deshmukh, PhD, MPH, Department of Public Health Sciences and Hollings Cancer Center, Medical University of South Carolina in Charleston, South Carolina. It was published online on June 17 in Annals of Internal Medicine.
LIMITATIONS:
This study assumed perfect adherence to all screening, diagnosis, and follow-up treatments, which may not reflect real-world conditions. In 2019, only 5% of people with HIV in the US had been screened for anal cancer in the preceding 12 months, likely due to the absence of consensus recommendations and limited high-resolution anoscopy capacity. Additionally, in settings with available screening resources, treatment uptake was poor and attrition during surveillance was common, which may alter the overall effectiveness and relative harm-to-benefit ratios of screening strategies.
DISCLOSURES:
This study was supported by the National Cancer Institute of the National Institutes of Health. The findings and conclusions contained in the study do not necessarily reflect the positions or policies of the National Institutes of Health.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Source link : https://www.medscape.com/viewarticle/anal-cancer-screening-cost-effective-hiv-positive-men-who-2025a1000g5h?src=rss
Author :
Publish date : 2025-06-17 12:02:00
Copyright for syndicated content belongs to the linked Source.