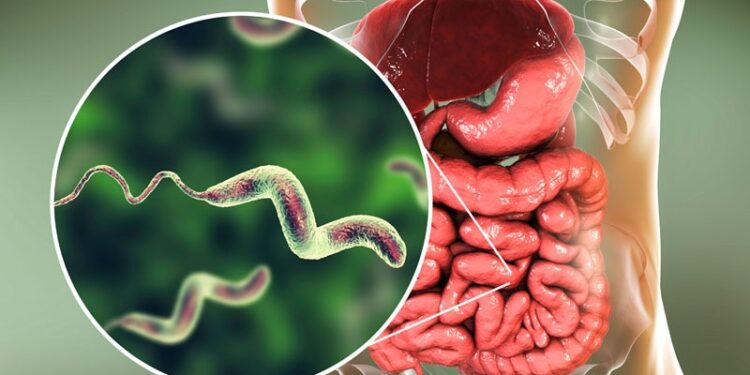
European surveillance data has revealed that Campylobacter bacteria in humans and animals and some strains of Salmonella continue to be highly resistant to widely used antimicrobials.
The two genera of bacteria are the most common causes of gastrointestinal infection in humans in Europe.
The data were revealed in a new report by the European Centre for Disease Prevention and Control (ECDC) and the European Food Safety Authority (EFSA), which found that Campylobacter are highly resistant to the commonly used fluoroquinolone, ciprofloxacin; designated by the World Health Organization as critically important for treating humans. This means that fluroquinolones can no longer be recommended for treating Campylobacter infections, according to the report.
Therese Westrell, PhD, principal expert of food- and water-borne diseases at the ECDC and a contributor to the report, told Medscape Medical News that they should probably also not be used to treat some strains of Salmonella.
Instead, azithromycin or erythromycin, both macrolide antibiotics, can be used to treat Campylobacter infections. Azithromycin can also be used as a last resort to treat Salmonella infections.
The ECDC and EFSA analyzed data reported in 2023 by the 27 European Union (EU) member states, the United Kingdom, Iceland, Norway, Montenegro, the Republic of North Macedonia, and Switzerland on antimicrobial resistance in bacterial isolates from humans, food-producing animals, and food. Resistance calculations for some bacteria-drug pairs were missing for some countries.
Among humans, the focus was on different strains of Campylobacter and Salmonella.
Campylobacter Highly Resistant to Ciprofloxacin
The two main Campylobacter species responsible for human infections are C jejuni and C coli. The report found that, across the EU, 71.9% and 75% of C jejuni and C coli isolates from humans, respectively, were resistant to ciprofloxacin.
Antimicrobial resistance in these bacteria varied significantly between countries.
While 28% and 16.7% of C jejuni and C coli isolates in Ireland, respectively, were resistant to the drug, the same was true for 97.5% and 100% in Lithuania.
Many factors may explain the wide variance in resistance between countries and isolates for the same drug, noted Westrell. These include differences in sampling strategies and antimicrobial use in food-producing animals, as well as statistical distortion from foodborne outbreaks.
The report further found that, across the EU, resistance to erythromycin remained low among C jejuni and C coli isolates, at 0.8% and 6.7%, respectively. Combined resistance to ciprofloxacin and erythromycin, considered critically important in the treatment of campylobacteriosis, was similarly low for both genera.
The report also tracked antimicrobial resistance trends between 2014 and 2023. While C jejuni isolates from Estonia and Spain and C coli isolates from Germany became more resistant to erythromycin over time, 10 countries saw significant declining trends.
“The decline in macrolide resistance in Campylobacter is primarily due to strong antimicrobial stewardship and reduced antibiotic use in both human and veterinary medicine,” said John MacSharry, PhD, senior lecturer in virology and immunology at University College Cork, Cork, Ireland, speaking to Medscape Medical News. He was not involved in the report.
EU bans on antibiotic growth promoters in 2006, restrictions on macrolide use in poultry farming, and reduced macrolide prescriptions for humans all played a key role in declining resistance, he added.
Salmonella Resistant — But Not as Much
The report also revealed that, across the EU, 21% of Salmonella isolates from humans were resistant to ampicillin, sulfonamides, and tetracyclines.
Meanwhile, just 2.3% of Salmonella isolates expressed high-level resistance to ciprofloxacin. S kentucky stood as an outlier, with 83.7% of its isolates showing high-level resistance, noted the report.
Salmonella isolates generally had low resistance to last-line antimicrobials, with 0.9% and 3% showing resistance to azithromycin and tigecycline. Combined resistance to ciprofloxacin and cefotaxime was also low, standing at 1.1%.
“A significant decline in ampicillin and tetracycline resistance in S typhimurium isolates from
humans was observed in 14 and 12 countries, respectively,” said Bruno Silvester Lopes, PhD, lecturer in microbiology at Teesside University, Middlesbrough, England, told Medscape Medical News. He was not involved in the report.
Lopes noted that the trend was largely driven by declining resistance in isolates from pigs and cattle younger than 1 year of age, which are key reservoirs for the bacteria.
“The reduction may reflect changes in antimicrobial use policies, including restrictions on tetracyclines and penicillins in food-producing animals. Also, vaccine protection against Salmonella species is now available in at least 12 European countries, which might have a role in prevention of disease in these animals,” he added.
MacSharry added that replacing penicillins and tetracyclines with newer antibiotics in human medicine also reduced selection pressure for resistant Salmonella, and that stronger surveillance and control of multidrug-resistant S typhimurium helped limit the spread of highly resistant strains.
“These trends highlight the effectiveness of antimicrobial stewardship,” he said, adding that resistance can decline when unnecessary antibiotic use is curtailed, preserving drug efficacy for the future.
MacSharry and Lopes reported no relevant financial relationships.
Annie Lennon is a medical journalist. Her writing appears on Medscape, Medical News Today, and Psych Central, among other outlets.
Source link : https://www.medscape.com/viewarticle/antibiotic-resistance-continues-some-variation-2025a10005wt?src=rss
Author :
Publish date : 2025-03-11 11:18:00
Copyright for syndicated content belongs to the linked Source.