As patients transition to geriatric care, considerations about treatment-related side effects, polypharmacy, comorbidities, and life expectancy become paramount.
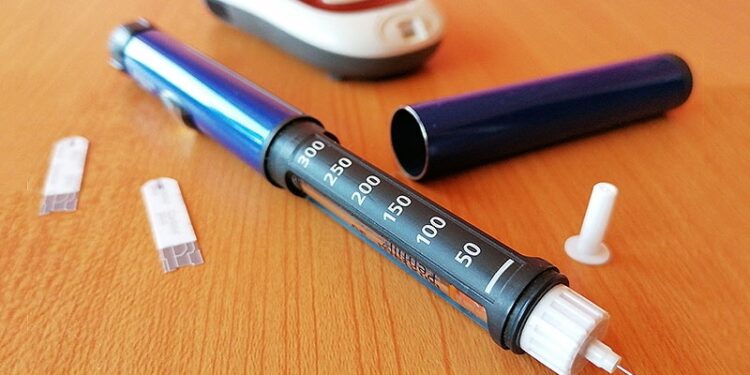
This is especially true for older adults with type 2 diabetes (T2D) taking insulin and/or sulfonylureas — steadfast older drugs that provide excellent glucose control but carry significant risk for iatrogenic hypoglycemia — one of the leading preventable treatment complications in this patient population.
“We have a gap in how we think about diabetes care because the paradigm is about tight glycemic control and blood pressure and cholesterol control. But that falls apart as patients grow older into their 70s, 80s, and 90s, and the goals of treatment start to change,” said Richard Grant, MD, MPH, research scientist with Kaiser Permanente Division of Research in Northern California. “There’s a need to switch the paradigm of tight control for everyone to control that depends on the patient,” he said.
The key, he said, was to improve diabetes medication deprescribing (ie, reducing the dose and/or frequency, or discontinuing potentially harmful medications).
Grant is the lead author of a randomized study assessing two strategies for improving diabetes medication deprescribing in 450 primary care patients (mean age, 79 years; SD, 4.0 years), with a mean hemoglobin A1c of 7.5% (SD 1.1%). One group of primary care practitioners received academic detailing involving evidence- and case-based teaching sessions, and study participants assigned to them received an attention control healthy lifestyle handout (eg, screening reminders, diet).
The second strategy entailed academic detailing plus patient pre-visit activation, which involved an educational handout to prepare patients assigned to these doctors for upcoming clinical visits. In the study, the content was based on a one-page medication review to help them discuss medication goals with their providers.
“The direct intention of the intervention was to encourage deprescribing. We demonstrated that at 6 months follow-up, involving the patient in these discussions led to almost twice as much deprescribing (15.8%) as academic detailing alone (9%),” said Grant.
Severe Hypoglycemia in Elderly Patients
Not only is iatrogenic hypoglycemia is considered the leading preventable, treatment-related complication, but it has been associated with significant negative health complications.
“It can cause confusion, people can get into accidents and injure someone else or themselves,” said Pankaj Shah, MD, endocrinologist at Mayo Clinic in Rochester, Minnesota. “Low blood sugars can also cause cardiac arrhythmias and sudden cardiac death,” he said.
“The risk of dying after an initial episode of hypoglycemia is very high,” Shah said. “It foretells that it is going to happen again down the line or something else is going to happen.”
Patients with T2D who land in the hospital with severe hypoglycemia also have increased risks for in-hospital mortality, repeated hospitalizations, and poor metabolic control.
In the study, the addition of the pre-visit patient intervention did not have much of an impact on self-reported hypoglycemia rates which, at 6 months, were similar between the two arms). However, the strategy was associated with fewer (albeit not statistically significant) iatrogenic hypotension-related hospitalizations at 6 months.
Determining the ‘Who’ of Deprescribing
There is no cut-and-paste pathway or algorithm for the optimal deprescribing strategy, according to Grant.
But the study findings showed “that involving the patient in the discussion led to almost twice as much deprescribing as academic detailing alone,” he said, thereby highlighting the importance of shared decision-making.
“Determining an individualized A1c target in older adults is not straightforward,” said Nestoras Mathioudakis, MD, MHS, associate professor in the Division of Endocrinology and co-medical director of diabetes prevention and education at Johns Hopkins Medicine in Baltimore.
Mathioudakis explained that the American Diabetes Association guidelines recommend A1C targets of less than 8% for older adults with complex health issues and offer no guidance on A1C targets for older adults with very complex health issues and limited life expectancy.

Part of the challenge is that people over the age of 75 have varying functional status and health status overall. For an active, healthy 76-year-old with very few comorbidities and a long-life expectancy, the benefits of continued glycemic control may outweigh the risks of hypoglycemia, he said.
The question then becomes, “Who do I de-intensify? How do I select that person? I think that we lack rigorous evidence and tools to guide us in making that decision,” said Mathioudakis.
“Let’s put it this way,” added Shah. “we should definitely deprescribe in patients who’ve had complications from their drug even once, whose blood glucose is so well controlled that they are likely to develop hypoglycemia or drug complications, and/or whose life expectancy is below 15-20 years,” he added.
Clinical Considerations
Though a pre-visit patient activation strategy might help promote medication discussions and prompt practitioners to consider deprescribing, the largest challenges often lie with patients themselves. In a related editorial, lead author Scott J. Pilla, MD, MHS, assistant professor at Johns Hopkins Medicine, noted the hesitancy that older adults with diabetes might feel toward deprescribing.
“There are patients who’ve had decades of being conditioned to get an A1C less than 7%, so there’s resistance to change associated with the fact that practice patterns have changed. It’s not an easy conversation to have with patients,” said Mathioudakis.
“If we come from [these discussions] from two angles — newer medications, SGLT-2 inhibitors, GLP-1 receptor agonists, and dual GLP/GLP-1 receptor agonists are the most effective from a cardiovascular perspective and are less dangerous from a hypoglycemic perspective — it’s then easier to justify the switch,” he said.

“But there’s also a debate as to whether they are appropriate in older patients, who have lower body mass index to begin with. So, we need to assess for hypoglycemia, perhaps, leveraging data from continuous glucose monitors in an automated fashion and using alerts in electronic medical records to prompt discussions,” he said.
Getting to these discussions, especially within primary care settings where time is tight, is the elephant in the room.
“We have to reassess whether the patient needs to continue on those medicines, reduce their numbers and simplify regimens, especially as life expectancy declines and risks of side effects start showing up,” said Shah.
“Deprescribing should be thought of pretty much every year, if not more often, especially if there are side effects,” he said.
The study was funded by the Patient-Centered Outcomes Research Institute. Grant, Shah, and Mathioudakis reported having no relevant financial relationships.
Liz Scherer is an independent health/medical journalist. She frequently covers news and features for Medscape Medical News and Medscape Global.
Source link : https://www.medscape.com/viewarticle/should-you-consider-deprescribing-older-type-2-diabetes-2025a1000jpq?src=rss
Author :
Publish date : 2025-07-25 11:45:00
Copyright for syndicated content belongs to the linked Source.