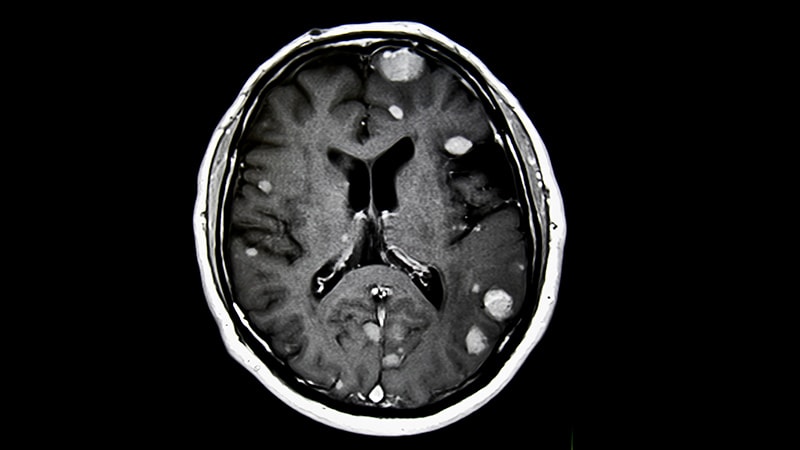
Evaluating the central vein sign (CVS) with a 35% proportional threshold on 3 Tesla (3T) MRI offers high sensitivity and specificity in distinguishing multiple sclerosis (MS) from migraine, a new study showed.
Researchers also found that analyzing six randomly selected CVS-positive (CVS+) lesions provided greater diagnostic accuracy than assessing three, offering a more efficient approach for clinical decision-making.
Investigators led by Giulia Silvestri, MD, Department of Neuroradiology at Ospedale Galliera in Genoa, Italy, prospectively enrolled 70 patients with MS and 50 age- and sex-matched patients with migraine, the most frequent neuroimaging MS mimic.
Among the 2766 MS lesions analyzed, 68.3% were CVS+ compared with just 16.1% of the 579 lesions in the migraine cohort. In both groups, the highest proportion of CVS+ lesions were located in the deep/subcortical region, accounting for 54.3% in MS and 63.4% in migraine.
The study was published online on January 20 in Headache.
Previous migraine studies by Solomon and colleagues and Cagol and colleagues revealed CVS+ rates of 19% and 8%, respectively, in the deep/subcortical region.
Silvestri and colleagues hypothesized that the increased sensitivity of their MRI technique, which combines three-dimensional (3D) T2 fluid-attenuated inversion recovery sequencing with high-resolution 3D T2*, known as echo-planar imaging (EPI), in a single image — may have enhanced visualization of venules within small deep/subcortical white matter (WM) lesions in patients with migraine.
This situation possibly elevated these patients’ CVS counts while potentially excluding multiple vein configurations within larger periventricular WM lesions in patients with MS, authors noted.
Compared with conventional susceptibility-weighted imaging, the investigators added, high-resolution 3D T2*-EPI better identifies the optimal CVS threshold for discriminating between MS and non-MS conditions. Using an optimized 0.65 mm isotropic voxel 3D T2*-EPI sequence, the CVS threshold that most reliably differentiated MS from migraine was 35.0% (sensitivity 97.1%; specificity 85.7%).
Further Research Needed
Commenting on the research for Medscape Medical News, Stephen D. Silberstein, MD, professor of neurology and director of the Jefferson Headache Center at Thomas Jefferson University in Philadelphia, said the investigators’ post-scan exclusion of eight patients with migraine who lacked WM lesions — or 16% of this 50-patient cohort — may have exaggerated the proportion patients with migraine who had CVS+ WM lesions. Silberstein was not involved in the research.
Also commenting, Bruce Cree, MD, PhD, MAS, professor of neurology at the University of California, San Francisco, School of Medicine, said that based on the 35.0% cutoff’s 0.95 area under the curve, authors’ advocating for the 3T pulse sequence and technique to identify the CVS is reasonable.
For clinical expediency, researchers have previously suggested analyzing three or six CVS+ lesions regardless of brain location. In the present study, the select6 and select3 algorithms would have correctly diagnosed all patients with MS while misdiagnosing 2.4% and 25.9%, respectively, of patients with migraine as having MS.
The select6 method more effectively distinguishes MS from migraine, said Cree, because patients with MS tend to have more lesions in the juxtacortical and periventricular WM vs patients with migraine. Consequently, he said, identifying CVS+ lesions in MS is somewhat easier when evaluating a limited number of lesions.
Methodologically, added Cree, using a small case-controlled dataset, as authors did, is reasonable in research settings when patients’ underlying diagnoses are known. But typically, he said, the utility of a diagnostic tool must be validated in a larger, prospective dataset wherein underlying diagnoses are unknown.
“That’s the next step before you try to roll this out into clinical practice,” said Cree, who was not involved in the study.
Practice Changing?
Assuming the data are validated, said Cree, “then there’s the challenge of trying to convince radiologists to use a pulse sequence like this and to do the added effort of detecting the CVS+ lesions. And we know that making those types of changes in clinical practice is much more challenging than conducting research studies.”
Perhaps more importantly, said Silberstein, the researchers’ technique definitively diagnoses neither MS nor migraine. Silberstein said that from his perspective, the paper simply says that the more CVS+ WM lesions one finds on MRI — particularly if the proportion exceeds 35% in the select6 approach — MS is the most likely diagnosis.
If CVS+ lesions are absent or account for fewer than 35% of the sample, Silberstein added, “it could be migraine or anything else.” As such, he said the study’s methodology is unsuitable for diagnosing disorders other than MS.
Cree added that the paper mainly addresses radiologists’ ability to diagnose MS based on MRI scans without clinical information.
“In clinical practice,” he said, “one can distinguish between migraine, which is a headache phenomenon, and MS. As neurologists, we do this all the time.”
Clinical information and physical exam findings help neurologists to distinguish migraines from MS, said Cree, but such information is rarely available to radiologists at the time of an MRI scan.
Study authors reported no funding sources or relevant financial relationships. Silberstein and Cree reported no relevant financial relationships.
John Jesitus is a Denver-based freelance medical writer and editor.
Source link : https://www.medscape.com/viewarticle/can-central-vein-sign-distinguish-multiple-sclerosis-its-2025a10006ow?src=rss
Author :
Publish date : 2025-03-20 13:13:00
Copyright for syndicated content belongs to the linked Source.