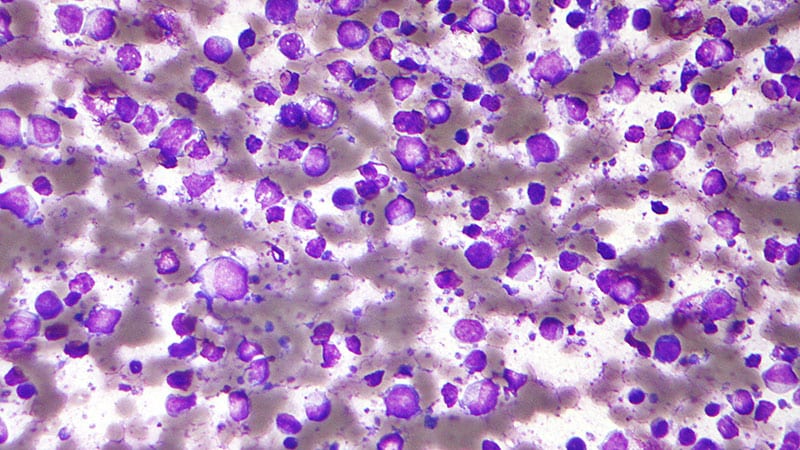
For patients with diffuse large B-cell lymphoma (DLBCL), the detection of circulating tumor DNA (ctDNA) following first-line treatment is independently predictive of disease recurrence and overall survival over 2 years, suggesting important prognostic value of the biomarker to improve upon standard assessment with PET-CT imaging.
“We demonstrated the prognostic value of ctDNA MRD [minimal residual disease] in first-line DLBCL cell patients [and that] ctDNA MRD provides independent evidence of residual disease beyond PET-CT,” said first author Steven Wang, MD, of Amsterdam UMC Location Vrije Universiteit, Amsterdam, the Netherlands, in presenting the findings at the 2025 American Society of Clinical Oncology (ASCO) Annual Meeting.
“These results support the integration of ctDNA MRD as a standard component of response evaluation in first-line DLBCL treatment,” he said.
The prognosis for long-term outcomes in DLBCL currently relies on PET-CT; however, key challenges with the approach include sometimes suboptimal sensitivity and specificity, with the potential to miss microscopic residual disease.
Liquid biopsy-based analysis of ctDNA, increasingly used in other cancers, meanwhile offers a radiation-free, non-invasive method for the assessment and monitoring of DLBCL.
To further investigate the biomarker’s prognostic benefits in DLBCL in a prospective context, Wang and colleagues evaluated data on 160 patients at more than 50 centers in the Netherlands and Belgium in the HOVON-902 trial.
Of the patients, most (79%) had stage 3 or 4 disease. All patients had been treated with curative-intent first-line therapy, with either R-CHOP or DA-EPOCH-R chemotherapy regimens.
In the assessment of ctDNA MRD, the investigators utilized the phased variant (PV) enrichment and detection sequencing (PhasED-Seq) assay, which targets unique “phased variant” alterations, or multiple mutations on the same DNA molecule.
The design boosts the assay’s sensitivity compared with other tests, which can have limitations such as error profiles of single nucleotide variants (SNVs).
Among the patients, most (90%) had DLBCL, with 9% having high-grade B-cell lymphoma and 1% with primary mediastinal large B-cell lymphoma.
In terms of the distribution of International Prognostic Index (IPI) risk level, 22% were low-risk, 29% low-intermediate risk, 27% high-intermediate risk, and 22% at high-risk. Patients’ median age was 67.5 years.
With 31 months of median follow-up in the cohort overall, the 24-month rates of progression-free survival (PFS) and overall survival (OS) were 74% and 86%, respectively.
The rates of PFS after 3 years were substantially higher for those who were MRD-negative at the end of treatment compared with those who were MRD-positive (85% vs 15%, respectively; hazard ratio [HR] 11.03; P < .0001), and 3-year rates of OS were also higher (92% vs 41%; HR, 7.38; P < .0001).
The findings show that “end-of-treatment ctDNA MRD is strongly prognostic for PFS and OS,” Wang said.
Higher cancer stage and IPI risk were associated with MRD positivity (both P < .05), and ctDNA was the most strongly prognostic of PFS (HR, 11.03), compared with end-of-treatment PET-CT results (HR, 5.31) or IPI level of risk (HR, 1.61).
Of patients who did not have a complete response based on PET results, MRD-positivity was likewise significantly prognostic for worse PFS at 3 years (PFS 4%) compared with those who were MRD-negative (PFS 64%), importantly suggesting the ability of MRD to adjudicate imaging results (HR for PFS, 6.78; P < .0001).
“End of treatment ctDNA MRD-positivity in patients without complete response have especially poor outcomes,” Wang noted.
All of the patients who did not achieve a complete molecular response and remained MRD-positive experienced a relapse.
The prognostic accuracy of ctDNA-MRD status was observed across subgroups, including based on the source of baseline sample (tumor vs plasma), best clinical response, IPI, sex, lactate dehydrogenase, stage, or extranodal disease.
The researchers also examined how ctDNA MRD status at the end of treatment correlated with the timing of response, and they found that 80% of patients who relapsed within a year of treatment had positive ctDNA MRD at the end of treatment, while only 22% of patients who relapsed after the first 12 months of first-line therapy had positive MRD.
“This distinction is important as early relapsers might be eligible for CAR T-cell therapy, and this demonstrates that end of treatment ctDNA MRD can reliably predict early relapses; however, long late relapses might require longitudinal MRD monitoring,” Wang explained.
“These data demonstrate the robust prognostic value of ctDNA MRD by PhasED-Seq in first-line DLBCL patients,” Wang said.
ctDNA Risk-Stratification Benefits Important
Discussing the research at the meeting, Mark Roschewski, MD, of the National Cancer Institute, Bethesda, Maryland, agreed that results on the timing of events were notably important.
“Now we can have a better understanding of when these events get captured [on ctDNA testing] and what we saw is that mostly these are early events,” said Roschewski, who recently co-authored a review of ctDNA as measurable residual disease in aggressive B-cell lymphoma.
Roschewski noted that the benefits of ctDNA are reflected in changes in National Comprehensive Cancer Network (NCCN) Guidelines, which indicate that ctDNA, using a sufficient test — such as PhasED Seq — does appear to be suitable as an alternative to invasive tissue biopsies for positive PET scans.
However, the most important thing that the research shows — which validates other findings — is that “these tests can actually risk-stratify patients who have positive as well as negative PET scans, improving upon our current definition of remission,” Roschewski added.
Ultimately, the findings show that “ultrasensitive ctDNA at the end of frontline therapy for large B-cell lymphoma is the most precise tool to define remission,” he said.
Not Ready for Prime Time?
However, for all of its promising benefits, a key concern expressed in the Q&A portion of the session was whether ctDNA could indeed be relied upon to replace a tissue biopsy in real-world practice.
For instance, while a positive PET scan and positive ctDNA MRD result could likely give clinicians confidence in moving ahead with second-line therapy, the approach may be less clear if a patient is PET-negative but MRD-positive.
“What I worry about is that [ctDNA] is prognostic, but not predictive, and with a relatively small dataset in this study, what are the implications in terms of overtreatment in that kind of situation?” one audience member noted.
“This is an important point,” responded Roschewski. “However, we should recognize that with the way things are done now, our PET scans have a positive predictive value of about 50%,” he said. “One of the concerns, and we see it in the data, is that these patients with a positive PET scan are getting second-line therapy when they don’t even have any active disease.”
“So, this is something that is already happening,” he explained.
Guidelines in such situations suggest either repeating the PET scan or the biopsy, hence delaying therapy.
“So, a negative ctDNA test could help you get information sooner,” Roschewski said.
“But would it improve patient outcomes?” the audience member pressed, getting to the issue of clinical utility.
“That’s something we don’t have data on yet,” Roschewski conceded. “I completely agree that this may not be ready for general clinical care without that data, but it may be fine in the context of a clinical trial for now.”
Roschewski noted that the good news is that “at least three clinical trials” are currently being planned to address the issues.
He noted that “we are able to [use this] in other hemolytic malignancies, but we have not gotten there yet [with DLBCL] and we need prospective trials to tell us what to do.”
The encouraging news, however, is “if we see success here, there is no reason to stop at large cell lymphoma. There are other curable lymphomas that we would like to test this in, and I think this could be a domino effect in which we start thinking about this all across therapies for a bunch of different lymphomas,” Roschewski said.
ctDNA Benefits in Early Disease Assessment Anticipated
Jane N. Winter, MD, professor of medicine, Division of Hematology/Oncology, Northwestern University, Chicago, Illinois, agreed that, with the data showing that ct-DNA is a powerful predictor of clinical outcome and can identify patients at high risk of relapse, “the big question is how we should use this information.”
For instance, “how important is it to identify refractory disease immediately at the end-of-treatment?” she said in an interview.
“I’m hopeful that ctDNA kinetics early in the course of therapy can help us identify patients for escalation of therapy,” said Winter, a past president of the American Society of Hematology. “Similarly, we might be able to use ctDNA to deescalate or abbreviate therapy.”
Ultimately, the results underscore that “ctDNA at the end of treatment is a powerful predictor of progression/relapse,” Winter said. “I’m very interested in using ctDNA as part of an early disease assessment.”
The study received funding from Gilead Sciences and the Liquid Biopsy Center. Wang, Roschewski, and Winter reported no relevant financial relationships.
Source link : https://www.medscape.com/viewarticle/can-new-biomarker-help-identify-high-risk-dlbcl-patients-2025a1000eqy?src=rss
Author :
Publish date : 2025-06-01 17:51:00
Copyright for syndicated content belongs to the linked Source.