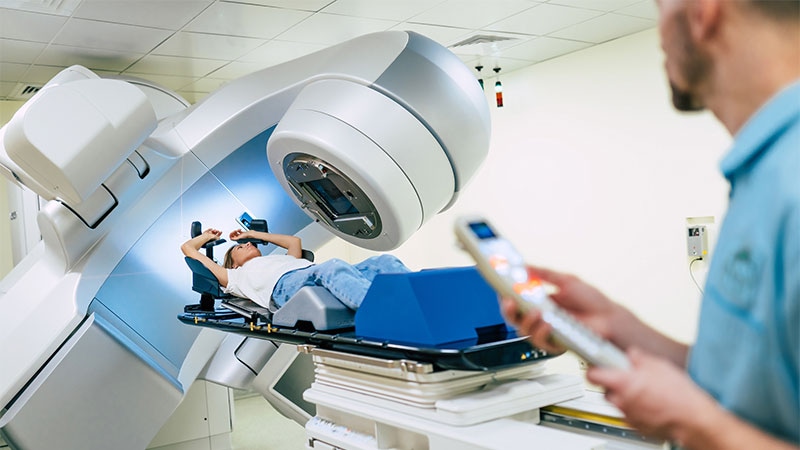
SAN ANTONIO — Postmastectomy chest wall irradiation is common for patients with early-stage breast cancer at intermediate risk for local-regional recurrence.
But new results call that practice into question. Findings from the SUPREMO trial found no difference in disease-free, metastasis-free, or overall survival at 10 years among patients who received irradiation and those who did not.
These results are important “for shared decision-making conversations between patients and clinicians, as many patients eligible for post mastectomy chest wall irradiation may not require the treatment,” said lead investigator Ian Kunkler, MBBS, a clinical breast oncologist at The University of Edinburgh, Edinburgh, Scotland. These patients may be able to avoid the risks for chest wall irradiation, such as chest wall pain, fibrosis, heart damage, and lung cancer, he added.
Once the findings are peer reviewed and published, the guideline groups will have to look at them “very seriously,” Kunkler said in a presentation at the San Antonio Breast Cancer Symposium (SABCS) 2024.
Trials from the 1990s did find a survival benefit for chest wall irradiation in patients with intermediate-risk breast cancer, which led to its support in treatment guidelines and widespread use.
However, those trials didn’t use optimal, more recently approved systemic treatments used in SUPREMO, which included taxanes, trastuzumab, anthracyclines, endocrine therapy, and other agents as appropriate, Kunkler explained.
The use of current standard-of-care treatments in this trial probably erased any survival benefits associated with radiation found in the older trials. In short, with modern systemic therapy, “adjuvant chest wall irradiation should be omitted in most patients meeting the eligibility of the SUPREOMO trial,” Kunkler said.
The international trial randomized 1607 women with intermediate-risk tumors to receive either chest wall irradiation (50 Gy in 25 daily fractions over 5 weeks or 40 Gy in 15 fractions over 3 weeks, n = 808), or to forgo radiation (n = 799) following mastectomy.
Intermediate risk was defined as tumors no larger than 50 mm with one to three positive axillary lymph nodes, tumors larger than 50 mm with no positive nodes, or node-negative tumors 20 mm-50 mm across (T2) with grade 3 histology and/or lymphovascular invasion.
Participants had surgical margins of at least 1 mm. One quarter of patients were node negative, just over 20% were Human Epidermal Growth Factor Receptor 2 positive, and slightly more than 10% were triple-negative. Neoadjuvant systemic therapy was allowed.
The researchers found that the 10-year overall survival was 81.4% with irradiation vs 82% without it.
Chest wall irradiation did lead to a reduction in locoregional recurrence — 20 chest wall recurrences without radiation vs 9 recurrences (hazard ratio, 0.45) — but the chest wall recurrence-free survival probabilities were almost the same between the groups — 98.8% for those who received radiation vs 97.1% for those who did not at the median follow-up time.
Although the results likely apply to most intermediate-risk patients, Kunkler cautioned that subgroup analyses by age, nodal status, and molecular subtypes are ongoing and unknowns remain for women who are not as well represented in the trial, including those with large, node-negative tumors and triple-negative breast cancer.
Study discussant Elinor Sawyer, MBBS, PhD, a clinical breast cancer specialist at King’s College London in London, England, echoed the caution.
“My take on SUPREMO is that I agree that we should not be giving postmastectomy radiotherapy for T2 node-negative patients who’ve had a mastectomy,” Sawyer said. “But I don’t think this can be generalized to all patients with one to three positive nodes, especially as only 12% of the patients in the trial had three positive nodes.”
The work was funded by the UK Medical Research Council, the European Organisation for Research and Treatment of Cancer, and others. Kunkler didn’t have any conflicts of interest. Sawyer disclosed receiving grants/research funding from Pfizer, Seagen, and IQIVIA.
M. Alexander Otto is a physician assistant with a master’s degree in medical science and a journalism degree from Newhouse. He is an award-winning medical journalist who worked for several major news outlets before joining Medscape Medical News. Otto is also an MIT Knight Science Journalism fellow. Email: aotto@mdedge.com
Source link : https://www.medscape.com/viewarticle/can-some-patients-safely-skip-postmastectomy-radiation-2025a10000fw?src=rss
Author :
Publish date : 2025-01-09 10:22:57
Copyright for syndicated content belongs to the linked Source.