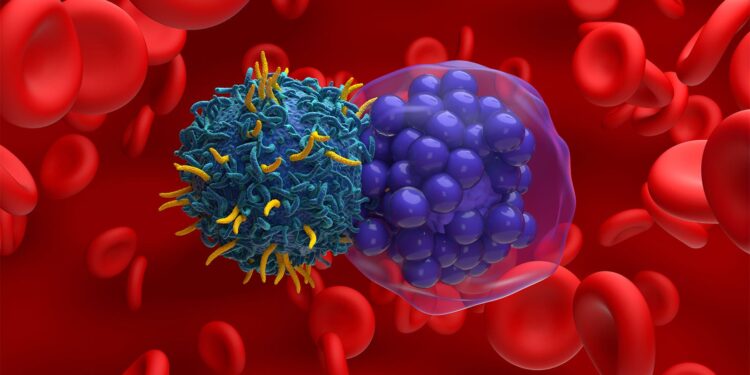
An investigational induced pluripotent stem cell-derived CAR natural killer cell therapy was well tolerated both as monotherapy and in combination with rituximab among patients with B-cell lymphomas, according to results from a phase I first-in-human trial.
For the 86 patients included in the study, the maximum tolerated dose of FT596 was not reached, and cytokine release syndrome (CRS) was reported in just one of 18 patients treated with monotherapy (maximum grade 1) and nine of 68 patients treated with the combination (six with maximum grade 1 and three with grade 2), reported Armin Ghobadi, MD, of the Washington University School of Medicine in St. Louis, and colleagues.
Furthermore, no dose-limiting toxicities occurred with monotherapy, and one occurred with the combination (consisting of prolonged grade 4 thrombocytopenia), and neither immune effector cell-associated neurotoxicity syndrome nor graft-versus-host disease were reported, they noted in The Lancet.
While the trial was not designed to evaluate efficacy, Ghobadi and colleagues said that responses were observed across B-cell lymphoma histologies among those treated with the combination, with an objective response rate of 54% and a complete response rate of 37%.
“FT596 appears to have a favorable safety profile compared with currently available immune cell therapeutics, with minimal cytokine release syndrome and no immune effector cell-associated neurotoxicity syndrome observed, allowing administration in the outpatient setting and, in combination with off-the-shelf availability, raising the potential for treatment of patients in community settings,” wrote Ghobadi and colleagues.
“Although this phase I study was not designed to definitively compare activity in specific diseases compared with available therapies, durable responses were observed, including in patients with aggressive lymphoma who had received previous autologous CAR T-cell therapy, an area of continued unmet need,” they added.
All patients with follicular lymphoma had a response (85% with a complete response), with a median duration of response of 16.9 months.
In addition, the objective response and complete response rates in 32 patients with large B-cell lymphomas were 38% and 25%, respectively, with a median duration of response not reached at a median follow-up of 9.1 months. Among 11 patients with large B-cell lymphomas other than de novo diffuse large B-cell lymphoma, objective response and complete response rates were 82% and 64%.
Moreover, patients who had undergone prior CD19-directed CAR T-cell therapy had a complete response rate of 30%, with all patients remaining in response at data cutoff (up to 26 months after the start of treatment).
In a commentary accompanying the study, Roman M. Shapiro, MD, and Rizwan Romee, MD, both of the Dana-Farber Cancer Institute in Boston, said FT596 addresses some of the limitations of allogeneic CAR T-cell therapy by “yielding both dose to dose and product to product consistency, shortening the manufacturing time, allowing for repeat dosing, and without causing graft-versus-host disease, severe cytokine release syndrome, or immune effector cell-associated neurotoxicity syndrome.”
They added that while the efficacy results need to be validated in a larger trial, “when considered alongside the safety profile of FT596, the results reported by Ghobadi and colleagues suggest that engineered [induced pluripotent stem cell]-derived CAR [natural killer] cells are a highly promising approach for allogeneic cell therapy of lymphoma.”
The study included 86 patients with B-cell lymphomas, 18 of whom received FT596 after conditioning chemotherapy without rituximab, and 68 who received FT596 combined with rituximab. These patients had a median age of 65.5 years, 74% were men, and 84% were white.
Of these patients, 30% had de novo diffuse large B-cell lymphoma, 17% had low-grade follicular lymphoma, 8% had transformed indolent non-Hodgkin lymphoma or grade 3B follicular lymphoma, 6% had high-grade B-cell lymphoma (double hit or triple hit), 14% had mantle cell lymphoma, 14% had Richter transformation, and 8% had other indolent lymphoma.
The median number of previous therapies was four, and 38% of patients had received previous CAR T-cell therapy.
The median time from FT596 infusion to CRS onset was 3.5 days, with a median duration of 3 days.
Grade 3 or higher infections were reported in 20% of patients across both regimen groups, and no patients discontinued treatment or died due to FT596-related adverse events.
Disclosures
The study was funded by Fate Therapeutics.
Ghobadi reported receiving consulting fees from Amgen, Atara, Bristol Myers Squibb, CRISPR Therapeutics, Kite, and Wugen, and research funding from Amgen, Genentech, Secura Bio, and Kite.
Several co-authors also reported relationships with industry.
The editorialists had no disclosures.
Primary Source
The Lancet
Source Reference: Ghobadi A, et al “Induced pluripotent stem-cell-derived CD19-directed chimeric antigen receptor natural killer cells in B-cell lymphoma: a phase 1, first-in-human trial” Lancet 2025; DOI: 10.1016/S0140-6736(24)02462-0.
Secondary Source
The Lancet
Source Reference: Shapiro RM, Romee R “iPSC-derived CD19 CAR NK cells for relapsed or refractory lymphoma” Lancet 2025; DOI: 10.1016/S0140-6736(24)02524-8.
Source link : https://www.medpagetoday.com/hematologyoncology/lymphoma/113755
Author :
Publish date : 2025-01-13 20:08:29
Copyright for syndicated content belongs to the linked Source.

![author['full_name']](https://newshealth.biz/wp-content/uploads/2025/01/CAR-Natural-Killer-Cell-Therapy-Shows-Promise-in-B-Cell-Lymphomas.jpg)