TOPLINE:
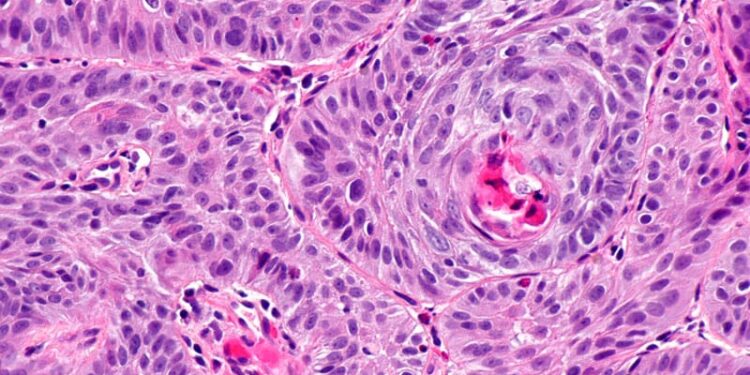
A recent analysis found that neoadjuvant chemoimmunotherapy led to higher 2-year overall survival and disease-free survival (DFS) rates than neoadjuvant chemoradiotherapy in patients with locally advanced esophageal squamous cell carcinoma (ESCC). Chemoimmunotherapy was also associated with lower overall recurrence and distant metastasis rates but a similar locoregional metastasis rate compared with chemoradiotherapy.
METHODOLOGY:
- While immunotherapy has improved outcomes in advanced esophageal cancer, its superiority over neoadjuvant chemoradiotherapy remains uncertain.
- This study included 1428 patients with locally advanced ESCC (median age, 63 years; 82.9% men)
- Patients received either neoadjuvant chemoimmunotherapy (n = 724), consisting of two cycles of immune checkpoint inhibitors every 3 weeks plus two cycles of platinum-based doublet chemotherapy, or neoadjuvant chemoradiotherapy (n = 704), which included a total radiation dose of 40.0-41.4 Gy in 1.8-2 Gy fractions for 5 days per week plus chemotherapy.
- The propensity score-matched analysis included 532 patients in each group.
- The study analyzed 2-year overall survival and DFS rates (primary endpoints); secondary endpoints included pathologic complete response and major pathologic response rates.
TAKEAWAY:
- Patients who received neoadjuvant chemoimmunotherapy demonstrated significantly higher 2-year overall survival (81.3% vs 71.3%; hazard ratio [HR], 1.57; P < .001) and DFS (73.9% vs 63.4%; HR, 1.37; P < .001) than those who received neoadjuvant chemoradiotherapy.
- The 2-year distant metastasis–free survival rates were also significantly higher in the chemoimmunotherapy group than in the chemoradiotherapy group (86.5% vs 74.8%; P < .001).
- The chemoimmunotherapy group exhibited a lower overall recurrence rate (23.7% vs 35.7%) and distant metastasis rate (13.5% vs 25.0%) than the chemoradiotherapy group.
- However, the chemoradiotherapy group did have a higher major pathologic response rate (71.8% vs 61.5% for chemoimmunotherapy), and both groups had comparable pathologic complete response rates (25.9% for chemoradiotherapy and 22.9% for chemoimmunotherapy) as well as similar rates of locoregional metastasis (20.9% for chemoradiotherapy vs 18.4% for chemoimmunotherapy).
IN PRACTICE:
“This study demonstrated that [ neoadjuvant chemoimmunotherapy] is associated with higher 2-year [overall survival] and DFS compared with [neoadjuvant chemoradiotherapy] in patients with locally advanced ESCC, primarily due to its ability to reduce the incidence of recurrence, especially for [distant metastasis],” authors of the study wrote.
“These excellent survival data reported by Guo et al provide strong motivation for prospective evaluation” of neoadjuvant chemoimmunotherapy in ESCC as well as in esophageal adenocarcinoma, Jessica S. Donington, MD, MSCR, University of Chicago, Chicago, said in an invited commentary.
SOURCE:
This study, led by Xufeng Guo, MD, Shanghai Chest Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China, was published online in JAMA Surgery, alongside an invited commentary.
LIMITATIONS:
This study was retrospective in nature, and data were collected from various centers, which may have introduced potential selection bias. This study used different immunotherapy and chemotherapy regimens, potentially introducing treatment heterogeneity. Additionally, the findings may not be fully applicable to esophageal adenocarcinoma.
DISCLOSURES:
This study was supported by grants from the National Clinical Key Specialty Construction Project, Program of Shanghai Academic/Technology Research Leader, and Cultivation initiative at the Basic Research Institute of Shanghai Chest Hospital. The authors reported no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Source link : https://www.medscape.com/viewarticle/chemoimmunotherapy-vs-standard-chemoradiotherapy-escc-one-2025a100076g?src=rss
Author :
Publish date : 2025-03-26 06:24:00
Copyright for syndicated content belongs to the linked Source.