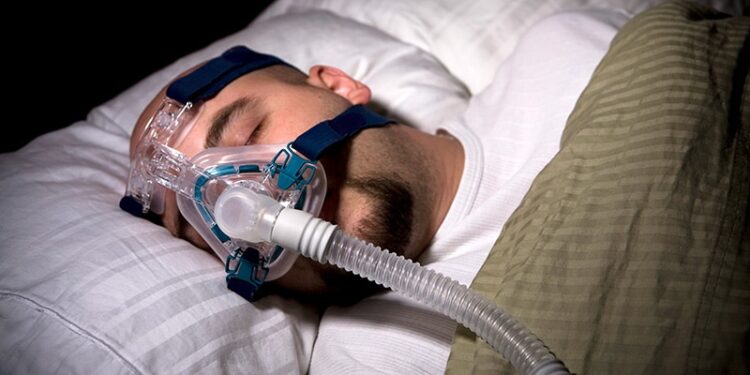
Obstructive sleep apnea (OSA) may raise the risk for Parkinson’s disease (PD), but early use of continuous positive airway pressure (CPAP) may mediate that effect, a large observational study showed.
“While our study found an increased risk of Parkinson’s disease, the good news is people can do something about it, by using CPAP as soon as they are diagnosed with the sleep disorder, [which] is encouraging,” study author Gregory D. Scott, MD, PhD, with the VA Portland Health Care System in Portland, Oregon, said in a news release.
The findings will be presented at the American Academy of Neurology (AAN) 2025 Annual Meeting in April.
Reduced Risk With Treatment
Some previous studies have suggested an association between OSA and PD, but few have examined the potential protective effects of CPAP.
Scott and colleagues evaluated OSA as a potential risk factor for PD and examined the impact of early vs late CPAP treatment by leveraging data from VA Corporate Data Warehouse spanning more than 20 years and more than 20 million veterans.
Early CPAP use was defined as CPAP within 2 years of OSA diagnosis and late use was defined as more than 2 years since OSA diagnosis.
Overall, nearly 1.6 million veterans had OSA and just over 9.7 million did not. The study team looked at rates of PD 5 years after a diagnosis of OSA.
After adjusting for age, sex, and health factors such as smoking, OSA was associated with a significantly increased risk for PD, with 1.8 extra cases per 1000 people at 5 years after OSA onset (P < .001).
The incidence of PD was similar in those who did not use CPAP and late users. However, early CPAP users had a significantly lower incidence of PD than nonusers, with a reduction of 2.3 cases at 5 years after OSA onset (P < .001).
The results suggest that OSA may be an “important, modifiable risk factor for PD, and potentially other synucleinopathies,” the study team wrote in their conference abstract.
“Future studies are needed to follow people more closely after receiving a sleep apnea diagnosis and over longer periods of time,” Scott added in the news release.
Novel Data With Clinical Implications
Commenting on the research for Medscape Medical News, Susheel Patil, MD, PhD, spokesperson for the American Academy of Sleep Medicine, noted that “most studies to date have suggested an association between OSA and PD, but have not necessarily examined whether CPAP use or other OSA treatments was associated with incidence reduction in PD.”
The current hypothesis for the potential association of OSA with PD holds that low oxygen levels seen with OSA can result in oxidative stress, which promotes neuroinflammation, which has a role in neurodegenerative disorders, said Patil, who is also affiliated with Case Western Reserve University and University Hospitals, both in Cleveland.
“In addition, oxidative stress may have a role in alpha-synuclein aggregation and cell death of dopaminergic neurons, which are seen in PD,” Patil said.
“The clinical implications for doctors counseling patients are to be mindful of risk factors for OSA in patients and guide them towards addressing when moderate to severe OSA is present. Early initiation of treatment might be beneficial in prevention of chronic diseases such as PD,” Patil said.
He urged caution, however, in interpreting the results.
“The study used electronic health records which may have limited data on individual behaviors or lifestyle factors that might be risk factors for PD. In addition, people who choose to start CPAP vs those that decline CPAP use may have differences in their health status and adherence to healthier lifestyles that may explain the reduction in PD seen in early CPAP adopters,” Patil explained.
“Further research, such as clinical trials, are necessary to clearly establish that treatment of OSA may prevent the development of PD,” he said.
This study was supported by the US Veterans Administration and the US Department of Defense. Scott and Patil had no related disclosures.
Source link : https://www.medscape.com/viewarticle/cpap-sleep-apnea-may-lower-risk-parkinsons-disease-2025a10005ra?src=rss
Author :
Publish date : 2025-03-10 08:06:00
Copyright for syndicated content belongs to the linked Source.