TOPLINE:
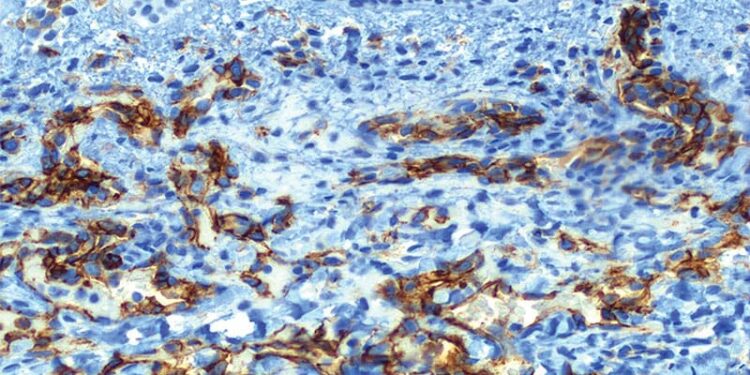
Direct immunofluorescence (DIF) microscopy showed a 15.5% positivity rate in pediatric patients and changed the clinical diagnosis in 16.7% of those cases.
METHODOLOGY:
- Researchers conducted a retrospective review of DIF data from 986 patients aged 0-18 years (mean age, 12 years) at the Mayo Clinic’s reference immunodermatology laboratory between August 2017 and November 2023.
- Biopsy sites included head and neck (cutaneous), head and neck (mucosal), trunk, pelvic region, upper extremities, and lower extremities.
- Results were classified as positive if characteristic immunofluorescence patterns were observed (pemphigoid pattern, pemphigus pattern, lupus pattern, dermatitis herpetiformis pattern, linear immunoglobulin A [IgA] bullous dermatosis pattern, vasculitis/vasculopathy pattern, or lichenoid tissue reaction pattern).
- During the same period, 40,859 DIF specimens from adults were also interpreted.
TAKEAWAY:
- The DIF positivity rate was 15.5% in children and 20.9% in adult specimens.
- IgA-predominant vasculitis was the most frequent DIF pattern in children (55.5%), followed by lichenoid tissue reaction (13.7%), pemphigoid disorders (7.2%), lupus (7.2%), dermatitis herpetiformis (5.2%), linear IgA bullous dermatosis (4.6%), pemphigus (3.3%), and non-IgA predominant vasculitis (3.3%).
- Of the 114 positive DIF patterns with a pretest diagnosis, researchers observed “relatively high” concordance between the clinical pretest diagnosis and DIF results (83.3%), but in 16.7% of cases, the initial clinical impression differed from positive DIF results. Linear IgA bullous dermatosis (100%) and dermatitis herpetiformis (100%) showed the highest concordance.
- Specimens from the lower extremities showed the highest yield of positive DIF compared with all other sites (19.7% vs 12.2%; P = .001).
IN PRACTICE:
The study findings showed that “similar thresholds for DIF biopsy are held” for pediatric and adult patients and “high concordance rates between positive DIF studies and clinical pretest diagnosis imply acceptable test specificity,” the study authors wrote. “The study demonstrated that DIF results provided information that changed the clinical impressions in a substantial percentage of cases, supporting the utility of DIF biopsy when immune-mediated dermatoses are clinically suspected,” they added.
SOURCE:
The study was led by Clint Christian T. Garbanzos, MD, Department of Pathology and Laboratory Medicine, MedStar Georgetown University Hospital, Washington, DC, and was published online on May 29 in Pediatric Dermatology.
LIMITATIONS:
Limitations included the retrospective design and lack of a negative analysis. False-positive and false-negative results could not be determined.
DISCLOSURES:
This study was supported by the American Society of Dermatopathology Mentorship in Dermatopathology Award. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Source link : https://www.medscape.com/viewarticle/direct-immunofluorescence-microscopy-helps-diagnose-2025a1000fw4?src=rss
Author :
Publish date : 2025-06-13 12:18:00
Copyright for syndicated content belongs to the linked Source.