[ad_1]
TOPLINE:
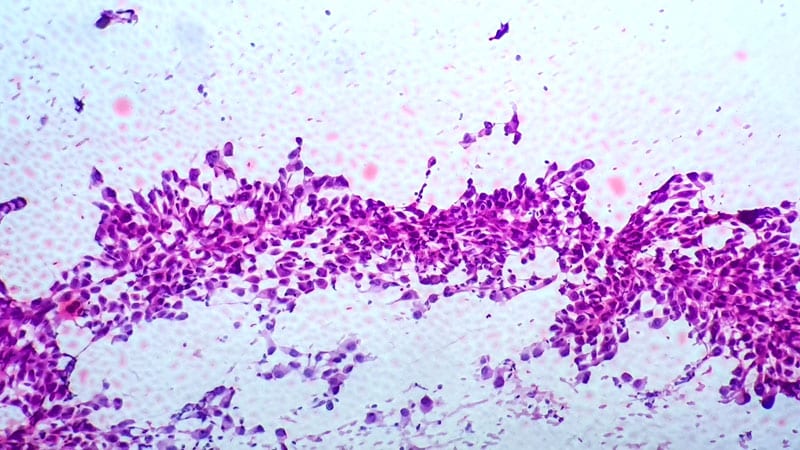
In patients with locally advanced non–small cell lung cancer (NSCLC), combining PET with invasive staging methods led to “relevant changes” of target volumes in 10% of cases, researchers reported. However, adding invasive staging methods to PET did not impact survival outcomes.
METHODOLOGY:
- Fluorodeoxyglucose (FDG) PET/CT is the standard for extracranial staging and target volume delineation in patients with newly diagnosed NSCLC. However, the role of invasive staging remains unclear.
- This secondary analysis of a prospective trial included 172 patients with locally advanced NSCLC undergoing concurrent chemoradiotherapy who were randomly assigned to undergo either FDG PET-CT with elective nodal irradiation or FDG PET-CT alone. The median follow-up duration was 41.1 months.
- Overall, 87 patients (50.6%) underwent at least one invasive staging modality, which included endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) and mediastinoscopy.
- Researchers evaluated 2752 lymph node stations noninvasively and 330 stations invasively via EBUS-TBNA or mediastinoscopy.
TAKEAWAY:
- The sensitivity of FDG PET-CT was 89.7% and specificity was 67.5%, based on histology as assessed by EBUS, while sensitivity was 82.6% and specificity was 66.7%, based on mediastinoscopy results.
- Invasive staging identified PET-negative but histologically positive lymph nodes in 10.3% of cases (13 lymph node stations in nine of 87 patients). Conversely, 36.8% of cases (67 lymph node stations in 32 of 87 patients) were PET-positive but negative on invasive staging.
- Survival outcomes, however, were unaffected by the number and type of staging procedures, with no correlation to overall survival, progression-free survival, or freedom from local progression, suggesting that invasive staging with EBUS-TBNA or mediastinoscopy did not impact outcome in these patients.
- Recurrence rates were low — six cases in the group undergoing FDG PET with elective nodal irradiation vs three in the group undergoing FDG PET alone — after 48 months of follow-up.
IN PRACTICE:
“In this unplanned secondary analysis of the [PET-Plan] trial, the use of 18F-FDG PET/CT in combination with EBUS-TBNA or mediastinoscopy resulted in relevant changes in target volume definition in 10% of patients, supporting the use of endoscopic mediastinal staging in combination with molecular imaging,” the authors wrote. “We did, however, see no effect of invasive staging on outcome in these patients with a low rate of isolated out-of-field recurrences.”
SOURCE:
The study was led by Andreas Rimner, Faculty of Medicine, University Medical Center, University of Freiburg, Freiburg, Germany, and was published online in International Journal of Radiation Oncology, Biology, Physics.
LIMITATIONS:
The study had a small sample size and potential selection bias as patients with higher PET-based nodal burden were more likely to undergo invasive staging. The original trial aimed to evaluate target volume reduction and was not powered to assess the impact of invasive mediastinal staging on outcome, particularly given the small number of patients with discrepant findings.
DISCLOSURES:
This analysis received funding from the German Cancer Aid. One author disclosed receiving consultant fees from Novartis, Roche, Telix, and Veraxa. Another author reported receiving support from the German Cancer Consortium and the Federal Ministry of Education and Research.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
[ad_2]
Source link : https://www.medscape.com/viewarticle/does-invasive-staging-improve-nsclc-survival-outcomes-2025a10006d7?src=rss
Author :
Publish date : 2025-03-17 12:05:00
Copyright for syndicated content belongs to the linked Source.