BBC Investigations, East Midlands
 BBC
BBCWeighing six stone and on the brink of organ failure, Charlotte Chapman-Hart is admitted to hospital in excruciating pain.
It’s assumed the former model and dancer has an eating disorder.
But Charlotte, who repeatedly denies she’s starving herself, has a rare disease.
She’s been prescribed a new pain relief medication, which should have been monitored by her GP and wasn’t. A side effect is rapid weight loss – but it’s been overlooked by those treating her.
Charlotte’s experience over the next three months would leave her adding post-traumatic stress disorder (PTSD) to the list of her symptoms. She now fears the care that she needs to stay alive.
“I think the hardest thing I’ve ever had to face is trying to convince people that I am of sound mind, and that what I’m telling you is the absolute truth,” says Charlotte, sitting in the garden of her home in Cuckney in Nottinghamshire.
“I told them that I’ve never had an issue with eating. I’m just not hungry. Things don’t taste the same.
“But rather than think differently, I was put into a diagnosis box that was wrong.”
Charlotte, who is now 32, has always lived in the same rented house with her mum and dad, who she relies on to look after her.
Since a young age, she’s loved dancing, starting classes when she was two.
Charlotte performed with the English Youth Ballet three times, between the age of eight and 16 after successfully auditioning.
“Dancing was my life, I was always known as Charlotte the dancer,” she says.
 Charlotte Chapman-Hart
Charlotte Chapman-HartWhen she was 13, she started experiencing chronic head and back pain. She said doctors blamed her training schedule and hormones.
“My mum took me to all these appointments explaining, ‘Charlotte will only complain if she’s really, really in pain’,” she says.
“But none of that was enough for people to do some diagnostic investigation.”
She continued dancing despite the pain, taking dance as one of her GCSEs at school and training with the Northern Ballet.
“Any time that I was in pain it was like, ‘it’s because you dance, it’s because of what you put your body through’,” she says.
 Charlotte Chapman-Hart
Charlotte Chapman-HartBy the time Charlotte graduated from university with a health and human sciences degree, she remembers being in physical agony almost constantly.
“It felt like an axe down the middle of my head,” she says.
“Sneezing and coughing created a huge amount of pain, I felt like my head was going to explode.”
At the age of 21, in 2014, Charlotte was diagnosed with chiari malformation type 1 – a condition in which part of the brain pushes down into the spinal canal – and syringomyelia, a rare neurological disorder.
She remembers the shock of hearing the results.
“He [the doctor] turned the monitor round and showed us the scans,” says Charlotte.
“It was like, ‘this is what you’ve got, this is how you spell it, this is what we’ve got to do’, and having just graduated, it was just like, ‘right, park that for a moment, we’re going to cut your head open’.”
 Chartlotte Chapman-Hart
Chartlotte Chapman-HartWhat is chiari malformation type 1 and syringomyelia?
According to the NHS, there are four types of chiari malformation, with type 1 the most common.
It is thought to affect one in 1,000 births, and can cause painful headaches, movement problems, dizziness and muscle weakness.
She also developed syringomyelia, which affects roughly eight in 100,000 people, in which cysts form on the spinal column.
Syringomyelia is one of an estimated 7,000 rare diseases under the UK Rare Diseases Framework.
Charlotte’s dreams of dancing were put on hold while she had emergency brain surgery.
She added: “I was really scared about the nature of it and I did genuinely have a fear of, am I going to survive this?”
Although no-one could have predicted what was to happen, she says there was no time to acknowledge that this was a significant moment in her life.
“Just to have a human kind of conversation with somebody would’ve been invaluable,” she says. “Because it does impact your sense of identity and nobody ever talks to you about that.”
 Charlotte Chapman-Hart
Charlotte Chapman-HartSurgery in 2015 to remove the base of her skull was successful. It alleviated the pressure and unblocked the cerebral spinal fluid so it could flow from the brain to her spine.
After recovering from surgery, Charlotte briefly returned to teaching dance, but had to stop completely due to worsening head and neck pain because of the surgery.
In November 2018, Charlotte unexpectedly started losing weight. By January, she’d lost a third of her body weight and was admitted to hospital with organ failure.
She didn’t know the new drug she’d been prescribed – which is used to treat epilepsy and migraine – could cause rapid weight loss, nor that it should have been monitored by her GP.
 Charlotte Chapman-Hart
Charlotte Chapman-HartBut when she was admitted to hospital in early 2019, doctors misdiagnosed her with an eating disorder.
During her three-month hospital stay, Charlotte says she experienced “domineering” and “dehumanising” care.
On one occasion, she says she was threatened with being sectioned if she didn’t admit to having an eating disorder. The whole experience, she says, caused her severe anxiety and PTSD.
“I felt like I was alone and had a lot of people and things to fear,” she says. “All of which were beyond my control to effect. I just felt very vulnerable.”
 Charlotte Chapman-Hart
Charlotte Chapman-HartAfter a brief recovery, a year later – in 2020 – Charlotte discovered that, when she got a Covid-19 jab – her prescribed pain medication had caused her severe weight loss.
A consultant later confirmed that she should have been closely monitored by her GP.
“That could have really, really made a difference to my quality of life, acknowledgement of that earlier on,” she says.
Then, in 2023, Charlotte suffered a sudden respiratory arrest and had to be resuscitated by neighbours.
She was never told what may or may not have caused it, but she believes things can change if patients like her are listened to.
“There’s been a lack of accountability,” she says. “I don’t want somebody to hold up their hands so that I can apportion blame.
“It’s so that we can learn. There’s no funding for research, but we are research. Our lived experience is research – capture it.”
 Charlotte Chapman-Hart
Charlotte Chapman-HartThis year, Charlotte became an ambassador for the charity Medics4RareDiseases, and is helping to raise awareness among health professionals.
It’s one of four priorities set out in the government’s Rare Diseases Action Plan, which aims to focus on faster diagnoses and better co-ordination of care.
“To contribute to something that could have the potential to really transform care is an incredible honour,” she says.
“It really makes all of the challenges, all the pain, absolutely worthwhile.”
 Dr Lucy McKay
Dr Lucy McKayIt’s real-life experiences like Charlotte’s that is being captured by Dr Lucy McKay, CEO of the charity.
“What people are asking for over and over again is to be listened to, is to be believed, is to be involved in their healthcare,” says Dr McKay.
“If technology, fast diagnosis and treatment alone were going to improve the lives of people with rare conditions, then we would already be fine.”
According to Medics4RareDisease, more than 3.5 million people in the UK live with rare conditions and often face the burden of constantly explaining themselves.
She adds Charlotte’s experiences are all too common, and can prove fatal.
 Charlotte Chapman-Hart
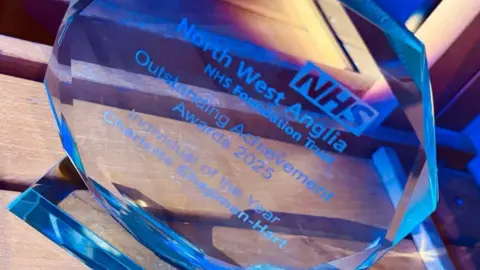
Charlotte Chapman-HartCharlotte now uses her role, as an assistant project manager for the North West Anglia NHS Foundation Trust – which she does from home – to share her experiences with clinicians.
This saw her recognised by the trust on 3 July as “individual of the year”, during an awards ceremony.
Despite Charlotte’s unpredictably debilitating symptoms, her ambition is to drive change.
She adds: “If I go to bed at night, knowing I couldn’t have done any more, then even if I don’t wake up the morning after, I’m content.”
The government says “it is clear that Ms Chapman-Hart’s care fell far below acceptable standards”.
“Our Rare Diseases Framework aims to improve awareness of rare diseases among health professionals and help patients get a faster diagnosis,” a Department of Health and Social Care spokesperson says.
“Our 10-year health plan will give more power and control to the patient.”
- If you have been affected by this story or would like support, then you can find organisations that offer help and information at the BBC Action Line
Source link : https://www.bbc.com/news/articles/c8d114rz07qo?at_medium=RSS&at_campaign=rss
Author :
Publish date : 2025-08-19 05:05:00
Copyright for syndicated content belongs to the linked Source.