Cancer guidelines have long recommended that women with suspected ovarian cancer be seen by a gynecologic oncologist, but a third of women with ovarian cancer in the United States never see one.
“They never make it to one of the doctors in this room,” said gynecologic oncologist Anna Jo Smith, MD, while speaking at a session of the Society of Gynecologic Oncology Annual Meeting on Women’s Cancers (SGO) 2025 in Seattle.
For women who do eventually see a gynecologic oncologist, it’s often only after seeing other specialists, which delays diagnosis and treatment.
“We know that treatment by GYN oncology is associated with at least 12 months longer survival for patients with ovarian cancer. Where you start matters,” said Smith, who practices at the University of Pennsylvania, Philadelphia.
At the meeting, Smith explained what she and her colleagues have done at their institution to address the situation and ensure that women with suspected ovarian cancer are seen by a gynecologic oncologist as quickly as possible.
In a pilot study, they added a “clinical nudge” to their center’s Epic records system that prompts clinicians to refer women with suspicious adnexal lesions — namely, lesions with an ovarian-adnexal reporting and data system ultrasound score of 4 or 5 on imaging — to gynecologic oncology.
Within 72 hours of imaging, clinicians receive a message in their inbox explaining that such lesions have at least a 10% chance of being cancer and that guidelines recommend referral.
A referral order is included with the message. If clinicians opt in, Smith and her colleagues handle the referral logistics. If clinicians choose not to refer, however, the clinicians are asked to explain why in a message. The goal was “to make not referring patients a little bit more difficult” than referring them, Smith said.
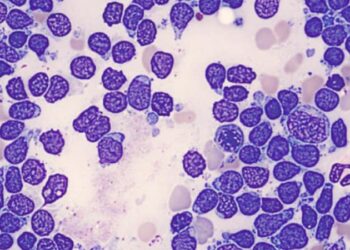
The approach seems to work. Although there were only 20 patients in the pilot, 75% of them were referred to gynecologic oncology, up from a historical baseline from their system’s records of 61%.
In addition, 92% of patients subsequently had surgery with a gynecologic oncologist, up from a baseline of 82%, and every patient who turned out to have cancer in the pilot had early stage 1 disease, compared with 77%.
Meanwhile, a third of the 20 clinicians who received the nudge said they would not have referred their patient to gynecologic oncology without it.
Given the results, a randomized controlled trial of the approach “is warranted,” Smith said.
The study “demonstrates a potentially practical and feasible intervention to improve health outcomes,” but it’s important that any future trial includes a diverse population to assess how the approach works across various patient populations, said study discussant Ann Oluloro, MD, a gynecologic oncologist at the University of Washington, Seattle.
Smith and her team are now thinking of rolling the nudge out for additional indications. “One of the things we are thinking about,” she said, “is how can we use this for uterine cancer or postmenopausal bleeding? How can you sort of adapt it to other situations?”
No funding source was reported for the work. Smith disclosed receiving a grant from GlaxoSmithKline and Oluloro reported receiving a grant from Merck.
M. Alexander Otto is a physician assistant with a master’s degree in medical science and a journalism degree from Newhouse. He is an award-winning medical journalist who worked for several major news outlets before joining Medscape. Alex is also an MIT Knight Science Journalism fellow. Email: [email protected].
Source link : https://www.medscape.com/viewarticle/electronic-medical-record-prompt-speeds-referral-gyn-2025a100070f?src=rss
Author :
Publish date : 2025-03-25 08:02:00
Copyright for syndicated content belongs to the linked Source.