Daratumumab and hyaluronidase (Darzalex Faspro, Johnson & Johnson) came a step closer to being approved for high-risk smoldering multiple myeloma (SMM) on Tuesday after the Oncologic Drugs Advisory Committee (ODAC) of the US Food and Drug Administration (FDA) voted that the benefits outweigh the risks.
However, the prospects of glofitamab (Columvi, Roche) for relapsed/refractory diffuse large B-cell lymphoma (R/R DLBCL) dimmed after the committee agreed with the FDA that the results of a trial, which was conducted largely in Asia, are not really applicable to patients in the United States.
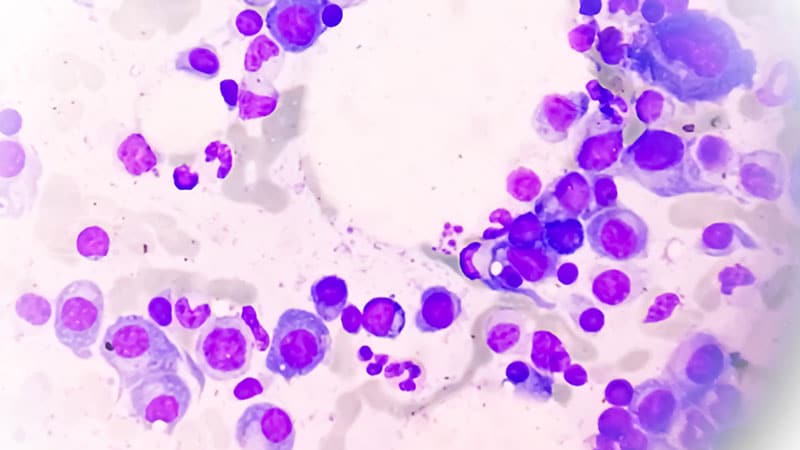
Daratumumab and hyaluronidase (DARA SC) is already on the US market as a standard first-line option for MM, but there’s currently no approved medication for SMM, an MM precursor. Standard treatment for SMM is either watchful waiting or referral to a clinical trial.
Glofitamab, meanwhile, has accelerated approval as monotherapy in the third or later lines for R/R DLBCL. Roche was hoping to move it to an earlier line of treatment in combination with gemcitabine and oxaliplatin for transplant-ineligible disease.
The FDA called the hearing because it had concerns about the trials supporting the two applications, AQUILA in the case of DARA SC and STARGLO for glofitamab.
STARGLO in the United States
STARGLO evaluated substituting glofitamab for rituximab on a background of gemcitabine and oxaliplatin for transplant-ineligible R/R DLBCL, not otherwise specified, following at least one line of systemic therapy. There was a statistically significant improvement in overall survival (OS), progression-free survival (PFS), and complete response (CR) with glofitamab across 274 patients.
The main concern the FDA had with the trial is that almost half of the patients were from Korea, Taiwan, and China, and there were only 25 US patients. Others came from Europe and Australia.
When the FDA compared outcomes of Asian vs non-Asian patients, it found significant differences. Despite a strong hazard ratio (HR) for OS benefit in Asia (HR, 0.39), there was a trend toward worse OS in Europe and the United States and in White patients, with similar trends for worse PFS and CR rates. The reasons aren’t clear.
“FDA is concerned by the lack of internal consistency observed in the STARGLO trial and how the results of the Asian region appear to be driving the overall trial results,” the agency said in meeting documents. “The low enrollment of patients in the US limits the agency’s ability to assess the applicability of the study results to a US patient population,” the FDA said in meeting documents.
“Furthermore, the FDA has identified multiple differences in patient-related, disease-related, and healthcare system–related factors between the non-Asian and Asian regional subgroup populations. Taken together, these issues raise uncertainty as to whether the results…are generalizable and applicable to a US patient population,” the agency said.
Among other concerns, the FDA also noted that rituximab/gemcitabine/oxaliplatin wasn’t a good comparator arm for US patients because the regimen is not commonly used in the United States, which might have contributed to low enrollment at US study sites.
Trial sponsor Roche highlighted the overall outcomes and that there’s an unmet need for additional DLBCL treatment options. Company representatives also said that outside of Asia, patients on glofitamab had a higher risk for disease than those on rituximab, and rituximab patients were more likely to subsequently receive new anti-lymphoma therapy like CAR T cells. It pinned the low US enrollment on COVID disruptions during the pandemic.
In the end, ODAC sided with the agency, voting 8 to 1 that the trial results are not applicable to US patients.
Echoing many committee members, panelist Heidi McKean, MD, community oncologist in Sioux Falls, South Dakota, said she voted that the trials wasn’t applicable “due to the inconsistencies in the results…and quite frankly, more patients in the US need to be looked at to prove efficacy and safety.”
Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence, said these issues in STARGLO aren’t uncommon.
“Unfortunately, if you take a look at all the oncology trials that come to us, only about 20% of the population is derived from the United States. We’d like to understand the reasons why sites are not enrolling in the United States. Potentially, that could be lack of interest because many times the control arms are not appropriate for a US population,” he said.
“This is going to be an area that the Oncology Center of Excellence is looking at quite closely. People are developing drugs for marketing in the United States, so it should address our interest here in the United States,” he said.
A Win for DARA SC
ODAC also considered the AQUILA trial, which randomized 390 patients with SMM at a high risk for progression to MM to either DARA SC or active monitoring for up to 3 years.
At a median follow-up of 65.2 months, the risk for disease progression or death was 51% lower with DARA SC than with active monitoring. At 5 years, PFS was 63.1% with DARA SC and 40.8% with active monitoring, and OS was 93.0% with DARA SC and 86.9% with active monitoring, although the trial was not adequately powered to demonstrate a significant improvement in OS.
The positive results were countered by a higher incidence of grade 3/4 treatment emergent adverse events with DARA SC, 40% vs 30%.
The FDA’s primary concern was that the trial, which was designed almost 10 years ago, used an outdated model to select patients at high risk for progression. With current risk models, only 41% of participants would be categorized as high risk, with 39% considered intermediate risk and 20% as low risk.
“This raises concerns regarding the applicability of the trial results to a population with high-risk SMM, as currently defined,” the FDA said in meeting materials.
Also, “while the trial met its primary PFS endpoint, there is uncertainty in the benefit of delaying progression to [multiple myeloma] in the absence of a significant improvement in OS. Additionally, the observed difference in progression was primarily due to differences observed in the biochemical or lab parameters,” not the onset of symptomatic disease, the FDA said.
Not all high-risk patients progress to MM, so the agency also had concerns about unnecessary treatment — particularly with the elevated risk for serious and high-grade adverse events with daratumumab.
“Given the limitations of the clinical meaningfulness of the efficacy findings and the toxicity observed with 3 years of treatment with Dara SC, there is uncertainty regarding the benefit-risk profile of Dara SC for patients with high-risk SMM,” the agency said.
Johnson and Johnson countered by emphasizing that all of the trials endpoints are positive, and that without an approved medication for SMM, patients are left powerless as they wait for a MM to emerge, something a commenter likened to “sitting on a ticking time bomb.”
Vincent Rajkumar, MD, myeloma specialist at the Mayo Clinic in Rochester, Minnesota, presenting on behalf of the company, also caught the attention of panelists when he said that high-risk SMM isn’t simply a benign precursor to MM, but rather cancer in itself, raising the stakes for early intervention.
“It is asymptomatic, but not premalignant. It is cancer. Genomically, [it is] indistinguishable from multiple myeloma,” he said.
In the end, the company’s arguments won the day. ODAC voted 6 to 2 that AQUILA provide sufficient evidence to support a favorable risk-benefit profile for DARA SC for SMM.
“The shift for me was thinking of smoldering multiple myeloma as a malignancy and allowing the physician and patient to look at this data and intervene earlier if they so choose,” McKean said.
Another committee member, Christopher Lieu, MD, gastrointestinal medical oncologist at the University of Colorado Cancer Center, Aurora, Colorado, agreed.
“I really want patients and providers to have the option to discuss this, to have the benefit-risk discussion. The conversation includes the fact that there are toxicities from this drug; that there’s a chance that you can prevent a life-altering fracture; that you might be able to prevent or delay at least the onset of treatment; that you might be able to delay or prevent an organ damage. I think that that is a conversation that I want patients and providers to have the option to have,” Lieu said.
However, this is going to lead to overtreatment. There has to be a predictive biomarker or some type of risk stratification to refine this high-risk group,” he said.
The FDA usually follows the advice of its advisory committees.
M. Alexander Otto is a physician assistant with a master’s degree in medical science and a journalism degree from Newhouse. He is an award-winning medical journalist who worked for several major news outlets before joining Medscape Medical News. Alex is also an MIT Knight Science Journalism fellow. Email: aotto@mdedge.com.
Source link : https://www.medscape.com/viewarticle/fda-advisory-daratumumab-wins-smoldering-myeloma-glofitamab-2025a1000cxm?src=rss
Author :
Publish date : 2025-05-22 13:28:00
Copyright for syndicated content belongs to the linked Source.