Anyone with fibromyalgia can tell you it hurts, but no one can yet explain what causes all those aches.
A study published in Pain Reports adds a new piece to the puzzle, showing spinal disinhibition — disruption of the spinal cord’s inhibitory systems that modulate pain signals — in people with fibromyalgia syndrome. The results suggest that spinal disinhibition could be a mechanism for generating pain in fibromyalgia.
These findings fit into much of the current thinking on chronic pain in people with fibromyalgia, says Roland Staud, MD, professor of medicine in the Department of Rheumatology at the University of Florida, Gainesville, Florida, who was not involved with this study.
“Regulation of sensitivity, including spinal cord sensitivity, is abnormal in these individuals,” he said.
Recent evidence points to fibromyalgia as a pain dysregulation disorder, although the causes of altered pain processing in the brain and spinal cord remain elusive.
“The reasons for this dysregulation at this point can only be speculated because no specific evidence has been accumulated that really is strongly related to these abnormalities,” Staud said.
Measuring Spinal Disinhibition
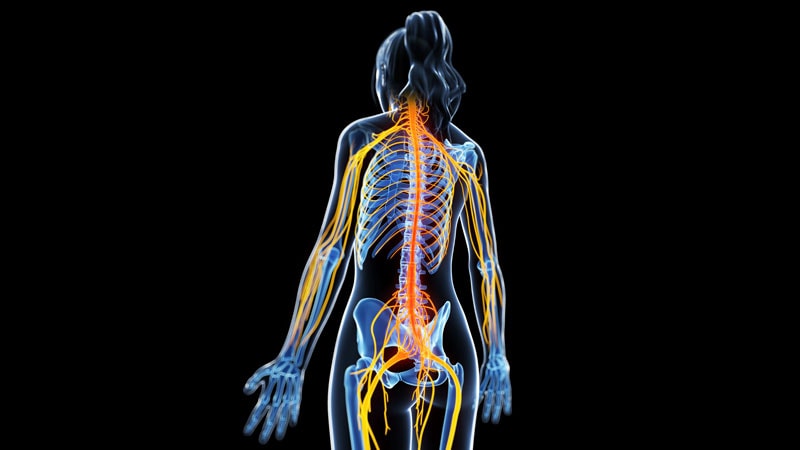
Your spinal cord’s pain processing circuits receive sensory inputs, feedback from your brain, and inputs from local neurons.
“What determines the output of those spinal circuits, the pain messages that are sent up to the brain?” asked Mike Hildebrand, PhD, professor in the Department of Neuroscience at Carleton University, Ottawa, Ontario, Canada, who was not involved with the study. “There are gas pedal mechanisms — excitation — and there are brake pedal mechanisms — inhibition — and anything that alters those competing processes will shift the balance of excitation-inhibition and the level of ascending pain signals.”
To measure spinal disinhibition in the new study, researchers used the Hoffman reflex (H-reflex) rate-dependent depression (HRDD) as a biomarker. They applied nerve-stimulating electrical pulses to the calves of 31 patients with fibromyalgia and 20 healthy control volunteers.
“The Hoffman reflex is basically an electrophysiological way of measuring your ankle jerk, your tendon reflex,” said study author Andy Marshall, MBChB, PhD, senior lecturer in pain neuroscience at the University of Liverpool, Liverpool, England. “Instead of tapping the tendon with a tendon hammer, we activate the sensory nerves because it’s a sensory and then motor loop that goes through the spinal cord.”
With normal spinal inhibition, the H-reflex response should have become smaller with repetition as the spinal cord regulates nerve activity and sensory information. However, people with fibromyalgia, especially those early in the course of their disease, had impaired HRDD. The H-reflex response did not get smaller like it did for healthy control volunteers.
The noninvasive HRDD measurement might someday be useful in studies testing early treatment in fibromyalgia, Marshall said. Identifying people with impaired central pain processing at an early stage may provide opportunities to optimize interventions. However, more research is needed to confirm the results of this small study.
“Prospectively looking at this going forward is going to be the key because we’re talking about a retrospective thing,” Marshall said. “Looking at when the diagnosis was and how long people have symptoms before can be a bit woolly, so I think that this needs to be confirmed with a prospective study.”
Staud noted that study participants were not asked to discontinue medications, including pain medications that are known to affect neural transmission and could affect study results.
Hildebrand said this study is exciting because there are so few preclinical models elucidating mechanisms in fibromyalgia. He hopes future fibromyalgia studies can test for sex differences in spinal disinhibition and maybe even include spinal cord imaging.
Spinal Disinhibition as a Future Treatment Target
While the causes of spinal disinhibition are not known, it can happen in neuropathic and inflammatory pain conditions, Marshall said. For example, spinal disinhibition has been seen in patients with diabetic neuropathy.
Here’s how things are supposed to work: The neurotransmitter gamma-aminobutyric acid (GABA) plays a key role in causing spinal inhibition, but whether GABA causes inhibition or excitation depends on the level of chloride in postsynaptic neurons. An ion transporter called potassium chloride cotransporter 2 (KCC2) is critical in maintaining chloride balance by moving chloride out of postsynaptic neurons.
In spinal disinhibition, postsynaptic neurons have altered intracellular chloride levels, possibly because of disrupted KCC2.
“If you have impaired or reduced KCC2, it changes the chloride balance within the postsynapse itself,” Marshall said.
There are already drugs in development that might specifically act upon the KCC2 transporter, so this is potentially a rich area for future study.
“It’s also been suggested that duloxetine, acting through its effect on 5HT2A [5-hydroxytryptamine (serotonin) 2A] receptors, may have a preferential effect on reducing spinal disinhibition by upregulating KCC2 and restoring chloride balance,” Marshall said.
In addition, brain-derived neurotrophic factor (BDNF) is a regulator of KCC2, so interventions aimed at BDNF could be a target for future research.
This study was funded by a grant from Versus Arthritis. The authors, as well as Staud and Hildebrand, reported having no relevant disclosures.
Source link : https://www.medscape.com/viewarticle/fibromyalgia-pain-might-start-spinal-cord-study-suggests-2025a100011c?src=rss
Author :
Publish date : 2025-01-16 11:32:35
Copyright for syndicated content belongs to the linked Source.