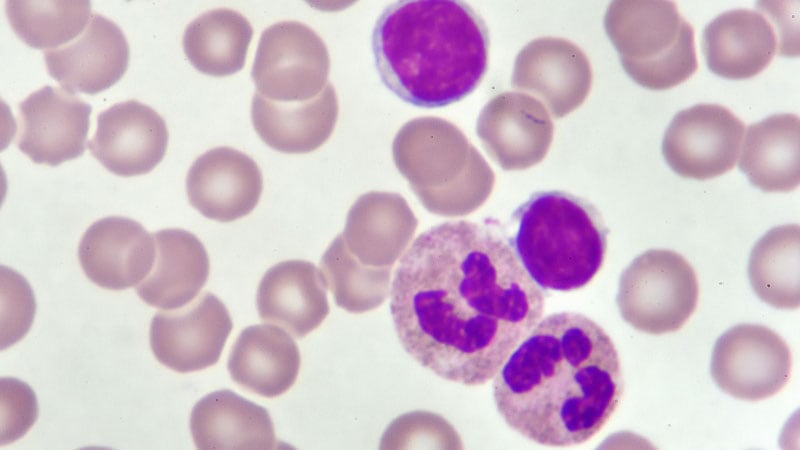
MILAN — Is chronic lymphocytic leukemia (CLL) progression primarily driven by genetic mutations or by external cues from the tumor microenvironment? Despite major strides in targeted therapies, CLL remains incurable, prompting renewed scrutiny of whether intrinsic genetic alterations or extrinsic cellular forces hold the key to more effective, lasting treatment.
This central question took the spotlight at the 2025 European Hematology Association (EHA) Annual Congress, sparking a lively debate among leading CLL researchers.
Most therapies have targeted intrinsic molecular features of leukemic cells, such as BCL2 and BTK. But the lack of robust responses to immunotherapy suggests that external factors such as the tumor microenvironment may also play a role.
“The debate dates back to at least 1999,” said session chair Silvia Deaglio, MD, PhD, director of the Immunogenetics and Transplant Biology Service, City of Health and Science of Turin, Italy in an interview with Medscape Medical News. “That year, two landmark papers showed that mutations in IGHV [immunoglobulin heavy chain variable region] genes were a favorable prognostic marker, supporting a genetic model. But those same studies also identified an unfavorable prognostic marker in a molecule linked to how CLL cells interact with their environment, suggesting a role for the microenvironment as well.”
Genetic Drivers Take Center Stage
Eugen Tausch, MD, PhD, researcher at the University of Ulm, Germany, argued in favor of genetics as the primary driver. “All CLLs have at least one genetic driver, and IGHV mutation status is a fundamental and stable biomarker,” he said.
This mutation status affects multiple cellular mechanisms, including immune evasion, anti-apoptotic signaling, and B-cell receptor function. It also modulates how cells respond to cues from their environment, reinforcing the need to consider IGHV when studying microenvironmental influences.
But IGHV is just one piece of the puzzle, Tausch added. More than 200 genetic drivers have been identified in CLL. Roughly 90% of cases harbor at least one gene mutation or chromosomal aberration that affects DNA repair, cell cycle regulation, metabolism, RNA processing, and intracellular signaling. “These alterations have clear clinical implications,” he said. “Resistance to BTK and BCL2 inhibitors often arises through mutations at the drug-binding site, establishing a direct link between genetics and therapy failure.”
Understanding and tracking clonal genetic evolution is thus key to risk stratification, treatment planning, and anticipating disease trajectory, he concluded.
The Microenvironment’s Role in Early Disease
Although CLL has long been seen as a genetically driven malignancy, new data suggest a more nuanced picture in which the tumor microenvironment influences early clonal dynamics.
“We know mutations drive disease progression, especially under therapeutic pressure, but the triggers of these mutations are less clear,” said John Gribben, MD, DSc, Hamilton Fairley Professor of Medical Oncology at Barts Cancer Institute, Queen Mary University of London, UK, who argued in favor of the microenvironment. Accumulation of mutations with age, oxidative stress, antigenic stimulation, and rare inherited factors have all been proposed, but these likely act in concert with tumor microenvironment signals to promote early clonal expansion, he explained.
In lymph nodes and bone marrow, CLL cells interact with a milieu of stromal and nurse-like cells, dysfunctional T cells, and dendritic cells, along with a variety of cytokines and chemokines. Recent studies have shown that early clonal evolution primarily occurs in lymph nodes and is associated with a suppressed T-cell inflammatory response. A small subpopulation of lymph node-activated CLL cells engages with the microenvironment to drive disease progression and possibly influence mutation patterns.
Moreover, therapies that disrupt microenvironmental interactions have shown efficacy by blocking B-cell receptor signaling and impairing chemokine-mediated trafficking.
Even while advocating for the microenvironment’s role, Gribben proposed a hybrid model. “Genetic lesions set the stage, but microenvironmental forces shape their emergence and survival. Early on, extrinsic factors dominate. Later, clonal evolution and genetic resistance take over.”
A New Paradigm of Coexistence
Both speakers emphasized the need to move beyond binary models of CLL progression. “The data support a dynamic interplay,” Deaglio told Medscape Medical News. “The long-term coexistence between leukemic cells and their environment in CLL alters both cell behavior and immune function.” She noted that the T-cell compartment becomes tolerogenic, showing expansion of regulatory T cells and memory effector cells, among other markers.
The debate also touched on the progression from monoclonal B-cell lymphocytosis to CLL and on Richter transformation, reinforcing the need for an integrated understanding of intrinsic and extrinsic disease drivers.
Deaglio underlined that researchers are now exploring whether treatment-resistant patients could benefit from new drugs or combinations and whether therapy could eventually be administered for fixed durations rather than continuously until progression.
“Progression is genetically driven,” said Deaglio. “But single-cell sequencing shows that some leukemic cells carry the features that enable future expansion a long time before the disease is diagnosed. Why some clones grow while others do not may depend on the environment they find themselves in.”
Gribben concluded, “To treat CLL effectively, and maybe reach a cure, we’ll need to combine immune-based approaches with current targeted therapies.”
Deaglio reported no relevant financial relationships. Tausch reported industry affiliations with AbbVie, BeiGene, Lilly, AstraZeneca, Roche, and Janssen-Cilag. Gribben reported research funding from AstraZeneca, BMS/Celgene, and Janssen; clinical trials with AbbVie, Celgene, Epizyme, Gilead, Genmab, Janssen, Merck, MorphoSys, Pharmacyclics, Regeneron, Roche/Genentech, and Takeda; consultancy for AbbVie, Amgen, AstraZeneca, BeiGene, BSM/Celgene, Janssen, Kite Gilead, and Takeda; and honoraria from AbbVie, AstraZeneca, BeiGene, BSM/Celgene, Janssen, Kite Gilead, and Novartis.
Cristina Ferrario is a molecular biologist and former researcher in molecular oncology at three institutes in Milan. She has a master’s degree in communication and health from the University of Milan and a master’s degree in cancer genetics from the University of Pavia, Italy. She has worked as a science journalist for more than 20 years.
Source link : https://www.medscape.com/viewarticle/genetics-or-microenvironment-what-drives-cll-progression-2025a1000gf8?src=rss
Author :
Publish date : 2025-06-19 14:08:00
Copyright for syndicated content belongs to the linked Source.