Patients with methotrexate-associated acute kidney injury (AKI) had better odds of kidney recovery when treated with glucarpidase (Voraxaze), researchers found.
Treatment with glucarpidase was associated with a 2.7-fold increase in the odds of kidney recovery compared with no glucarpidase treatment (adjusted OR 2.70, 95% CI 1.69-4.31) in data from multiple cancer centers, reported Shruti Gupta, MD, MPH, of Brigham and Women’s Hospital and Harvard Medical School in Boston, and colleagues, in Blood.
Patients treated with glucarpidase also had faster time-to-kidney-recovery (adjusted HR 1.88, 95% CI 1.18-3.33) and lower risks of grade ≥2 neutropenia (adjusted HR 0.50, 95% CI 0.28-0.91) and grade ≥2 transaminitis (adjusted OR 0.50, 95% CI 0.28-0.91) on day 7.
In a subgroup analysis, the magnitude of benefit from glucarpidase was higher among females compared with males. The odds of kidney recovery in treated patients was higher among those with stage 3 AKI, although this did not reach statistical significance.
“The study very clearly shows that glucarpidase improved the primary outcome of kidney recovery at time of hospital discharge, time-to-kidney-recovery, and potentially has benefits to other organs,” Gupta told MedPage Today.
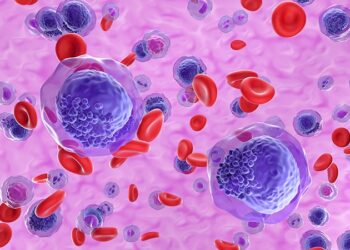
With its ability to penetrate the blood-brain barrier, methotrexate is an effective and widely-used chemotherapy, commonly used in patients with lymphoma or leukemia involving the central nervous system.
However, as with other chemotherapies, treatment with methotrexate often causes AKI, occurring in approximately 9% of patients. Methotrexate can also result in hepatotoxicity and neutropenia.
“A lot of these different chemotherapies that might be toxic to the kidneys haven’t had any antidotes available, whereas in this case with methotrexate, one actually exists regarding glucarpidase,” Gupta pointed out.
Glucarpidase — a carboxypeptidase enzyme that helps break down and remove methotrexate from the body — was approved by the FDA in 2012 to treat patients with toxic levels of methotrexate in their blood due to kidney failure.
“But when it was approved in 2012, that was based on very limited data,” Gupta noted. “We had chemical data — we knew glucarpidase rapidly reduces methotrexate in the blood,” but there haven’t been any studies that have rigorously evaluated whether glucarpidase actually improves clinical outcomes in patients with methotrexate toxicity, she added.
The result, said co-author David Leaf, MD, MMSc, also of Brigham and Women’s Hospital and Harvard Medical School, is that there has been “wide intrahospital variation in the use of glucarpidase.”
“It’s an expensive drug, and there has been very limited data that it actually results in a benefit to patients that is meaningful beyond the effect of lowering the levels of methotrexate,” he said. “Some hospitals use it a lot, and some don’t use it all, and there are conflicting guidelines on which patients should receive it, and all because of the lack of data.”
Conducting a randomized trial “would be impractical,” Gupta said. Instead, the researchers used observational data from 28 cancer centers to conduct a target trial emulation study to replicate a randomized clinical trial.
“[Target trial emulation] applies the core principles of [randomized clinical trials], including rigorous specification of inclusion and exclusion criteria, adjustment for detailed baseline characteristics to emulate random treatment assignment, and use of methodology to eliminate the potential for immortal time and other biases,” they wrote in Blood.
“Much in clinical research is done at the single center level, and that limits your sample size and generalizability,” Leaf observed. “The importance of doing these studies at a multicenter level is that providers at different hospitals do different things, and this provides a natural experiment that allows us to look at and leverage those data to emulate the conditions of a randomized clinical trial.”
The study included adults ≥18 years old who received high-dose IV methotrexate and developed methotrexate-associated AKI, defined as a ≥1.5-fold increase in serum creatinine within 4 days after initiation of methotrexate compared to baseline. Patients with end-stage kidney disease and those likely to die within 2 days at the time of methotrexate initiation were excluded.
The study included 708 patients (median age 64 years, 70% male); 29.5% were treated with glucarpidase and 70.5% were not. Of those treated with glucarpidase, 29.2% had primary central nervous system (CNS) lymphoma, 17.2% had acute lymphoblastic leukemia (ALL), and 50.2% had other lymphoma or leukemia. Of those not treated with the drug, 41.3% had primary CNS lymphoma, 8.2% had ALL, and 47.3% had other lymphoma or leukemia.
Glucarpidase-associated adverse events included nausea (5.7%), diarrhea (0.5%), and paresthesia (0.5%).
Glucarpidase-treated patients may have had more severe illness resulting in a possible underestimation of the magnitude of effect seen with glucarpidase, the researchers noted. They also had longer hospital stays, resulting in more time to recover.
In addition, serum creatinine was not assessed in a standardized way after hospital discharge, so time-to-kidney recovery (as a time-to-event analysis) could not be assessed beyond day 14.
Disclosures
The study was funded by BTG International.
Gupta was a scientific coordinator for the ASCEND trial, served as consultant for Secretome, Proletariat Therapeutics, and Alexion, and received research support from BTG International, Dana-Farber Cancer Institutes’s Wong Foundation, Janssen, and AstraZeneca.
Leaf received received research support from BioPorto, BTG International, and Metro International Biotech LLC, and served as a consultant for Sidereal Therapeutics, Casma Therapeutics, MexBrain, Entrada Therapeutics, and CardioRenal Systems.
Co-authors reported multiple relationships with industry.
Primary Source
Blood
Source Reference: Gupta S, et al “Glucarpidase for treatment of high-dose methotrexate toxicity” Blood 2025; DOI: 10.1182/blood.2024026211.
Source link : https://www.medpagetoday.com/hematologyoncology/hematology/113662
Author :
Publish date : 2025-01-06 20:56:43
Copyright for syndicated content belongs to the linked Source.

![author['full_name']](https://newshealth.biz/wp-content/uploads/2025/01/Glucarpidase-Improves-Outcomes-in-Methotrexate-Associated-AKI.jpg)