Glutamatergic medications showed promise in treating obsessive-compulsive and related disorders (OCRDs), especially obsessive-compulsive disorder (OCD), a systematic review and meta-analysis showed.
Across 27 trials, glutamatergic medications as monotherapy or added to selective serotonin reuptake inhibitors (SSRIs) showed a large effect size in improving OCRD symptoms (Cohen d -0.80, 95% CI -1.13 to -0.47) when the intervention group was compared with the control group, with low certainty of evidence, reported David Coelho, MD, MPH, of the Harvard T.H. Chan School of Public Health in Boston, and co-authors in JAMA Network Open.
For 23 trials that were OCD-specific, the mean reduction in scores on the 40-point Yale-Brown Obsessive Compulsive Scale (Y-BOCS) was statistically significant (mean difference -4.17 points, 95% CI -5.82 to -2.52) when comparing the two groups, with moderate certainty.
“The high heterogeneity and indications of publication bias identified in our study warrant a cautious interpretation of the findings. This variability likely reflects the diverse range of disorders, patient populations, and treatment approaches within the OCRD spectrum,” Coelho and colleagues wrote.
“However, in more homogeneous subgroups, such as those treated with medications such as topiramate or riluzole, we observed reduced heterogeneity, indicating that targeted treatments may yield more consistent and predictable outcomes,” they added.
Standard treatments, including SSRIs, clomipramine, and cognitive behavioral therapy, are often effective for OCRDs, the researchers pointed out. “However, approximately 60% of patients, particularly those with OCD, may not respond adequately to SSRIs as monotherapy, highlighting the need for novel therapeutic approaches,” they wrote.
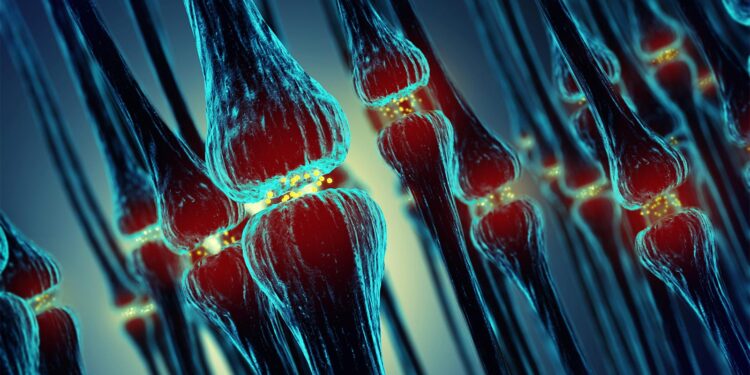
Glutamatergic medications modulate synaptic plasticity and neuronal excitability, potentially alleviating OCRD symptoms.
“Studies have expanded our understanding of OCRDs, revealing dysfunctions in neurobiological circuits involving the orbitofrontal cortex, anterior cingulate cortex, and basal ganglia. These findings have led to a growing interest in the role of the glutamatergic system in OCRDs,” Coelho and co-authors noted.
“Our results align with the emerging understanding of the role of the glutamatergic system in the pathophysiology of OCRD,” they added.
The researchers identified double-blind randomized controlled trials comparing glutamatergic medications with placebo for patients with OCRDs for any age, sex, gender, or degree of disease refractoriness.
The 27 trials in the meta-analysis included 1,369 participants with a mean age of 31.5 years. Most (65.6%) were women.
Four studies included children and adolescents, and 23 trials included adults. Most studies assessed OCD; two trials were about trichotillomania and two studied skin-picking disorder.
Main outcomes included scores on the Y-BOCS and its pediatric version, the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS). The clinician-administered Y-BOCS evaluates obsessive-compulsive symptom severity with total scores ranging from 0 to 40. Higher scores indicate greater severity.
Ten trials investigated N-acetylcysteine (NAC), four assessed memantine, three examined lamotrigine, three studied riluzole, and two evaluated topiramate. One study each assessed amantadine, glycine, L-carnosine, minocycline, and pregabalin.
“All studies reported minimal or no adverse effects,” Coelho and co-authors noted. “Among those that did, the adverse effects were generally mild to moderate, including nausea and vomiting, diarrhea, stomach and abdominal pain, and heartburn — all with NAC.”
Most studies (17 of 27) had low risk of bias, while seven had some bias concern, and three were considered to have high risk of bias.
Sensitivity analyses consistently showed an association between glutamatergic medications and symptom improvement, the researchers noted. Subgroup analyses showed no significant mean differences by population, refractoriness, augmentation strategy, risk of bias, or medication type.
“This systematic review differs from prior reviews by focusing on a broader population of OCRDs,” Coelho and colleagues observed.
“Previous reviews often targeted specific groups, such as individuals with OCD, or specific glutamatergic medications, such as NAC and memantine,” they continued. “Our analysis extends these insights by offering a more comprehensive evaluation across a wider spectrum of OCRDs and focusing on subgroup analyses based on important clinical characteristics.”
The meta-analysis was limited by relatively small trial cohorts and few studies evaluating some medications and some OCRDs, including skin picking disorder and trichotillomania, and no studies met the criteria for body dysmorphic disorder and hoarding disorder, the researchers acknowledged.
The analysis also was unable to assess dose-dependent effects due to dose escalation and inconsistent reporting.
“Promising therapeutic glutamatergic medications, such as ketamine and troriluzole, did not meet our inclusion criteria and warrant further research,” Coelho and co-authors added.
“Future research with larger sample sizes should focus on dose-dependent effects, additional OCRD subtypes, and novel glutamatergic treatments to enhance our understanding and treatment strategies.”
Disclosures
Researchers were supported by the Jorge Paulo Lemann Fellowship, the São Paulo Research Foundation, and the Center for OCD and Related Disorders at Massachusetts General Hospital.
Coelho and co-authors reported no conflicts of interest.
Primary Source
JAMA Network Open
Source Reference: Coelho DRA, et al “Glutamatergic medications for obsessive-compulsive and related disorders: A systematic review and meta-analysis” JAMA Netw Open 2025; DOI: 10.1001/jamanetworkopen.2024.52963.
Source link : https://www.medpagetoday.com/psychiatry/generalpsychiatry/113616
Author :
Publish date : 2025-01-02 17:43:28
Copyright for syndicated content belongs to the linked Source.