WASHINGTON, DC — Age-related neurodegenerative disorders — motor neuron diseases, demyelinating diseases, Alzheimer’s disease, and other proteinopathies — are at an “inflection point,” said researcher Andrea R. Merchak, PhD, with a fuller understanding of disease pathophysiology but an overall dearth of effective disease-modifying treatments.
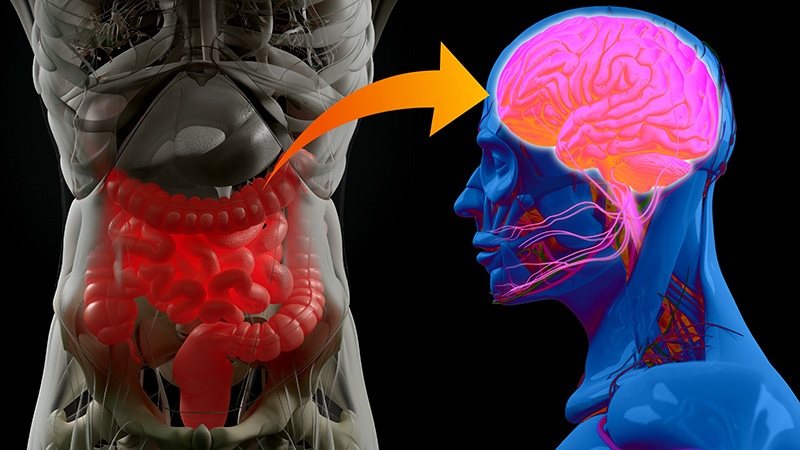
And this, Merchak said at the Gut Microbiota for Health (GMFH) World Summit 2025, is where the gut microbiome comes in. “The gut-brain axis is important to take into consideration,” she urged, both for gut microbiome researchers — whose collaboration with neurologists and neuroscientists is essential — and for practicing gastroenterologists.
“We are the sum of our environmental exposures,” said Merchak, assistant research professor of neurology at the Indiana University School of Medicine, in Indianapolis. “So for your patient populations, remember you’re not only treating the diseases they’re coming to you with, you’re also treating them for a lifetime of healthy [brain] aging.”
At the center of a healthy aging brain are the brain-residing microglia and peripheral monocytes, she said. These immune cell populations are directly influenced by blood-brain barrier breakdown, inflammation, and gut permeability — and indirectly influenced by microbial products, gastrointestinal (GI) function, and bacterial diversity, Merchak said at the meeting, which was convened by the American Gastroenterological Association and the European Society of Neurogastroenterology and Motility
“Many of us grew up learning that the brain is an immune-privileged site, but we’ve been establishing that this is fundamentally not true,” she said. “While the brain does have a privileged status, there are interactions with the blood, with the peripheral immune cells.”
Merchak coauthored a 2024 review in Neurotherapeutics in which she and her colleagues explained that the brain is “heavily connected with peripheral immune dynamics,” and that the gut — as the largest immune organ in the body — is a critical place for peripheral immune development, “thus influencing brain health.”
Gut microbiota interact with the brain via several mechanisms including microbiota-derived metabolites that enter circulation, direct communication via the vagus nerve, and modulation of the immune system, Merchak and her coauthors wrote. Leaky gut, they noted, can lead to an accumulation of inflammatory signals and cells that can exacerbate or induce the onset of neurodegenerative conditions.
As researchers better understand the role that GI dysfunction plays in neurodegenerative disease — as they identify microbiome signatures for predicting risk, for instance — there will be “opportunities to target the microbiome to prevent or reverse dysbiosis as a way to delay, arrest or prevent the onset and progression of neurodegenerative diseases,” they wrote.
At the GMFH meeting, Merchak described both ongoing preclinical research that is dissecting gut-brain communication, and preliminary clinical evidence for the use of gut microbiota-modulating therapies in neurodegenerative disease.
Support for a Gut-Focused Approach
Research on bile acid metabolism in multiple sclerosis (MS) and on peripheral inflammation in dementia exemplify the ongoing preclinical research uncovering the mechanisms of gut-brain communication, Merchak said.
The finding that bile acid metabolism modulates MS autoimmunity comes from research done by Merchak and a team at the University of Virginia, Charlottesville, Virginia, several years ago in which mice with experimental autoimmune encephalomyelitis (EAE) — an animal model of MS — were engineered for T cell specific knockout of the aryl hydrocarbon receptor (AHR). The AHR has been directly tied to MS, and T lymphocytes are known to play a central role in MS pathophysiology.
Blocking the activity of AHR in CD4-positive T cells significantly affected the production of bile acids and other metabolites in the microbiome — and the outcome of central nervous system autoimmunity. “Mice with high levels of bile acids, both primary and secondary, actually recovered from this EAE” and regained motor function, Merchak said at the GMFH meeting.
The potential impact of genetic manipulation on recovery was ruled out — and the role of bile acids confirmed — when, using the EAE model, gut bacteria from mice without AHR were transplanted into mice with AHR. The mice with AHR were able to recover, confirming that AHR can reprogram the gut microbiome and that “high levels of bile acid can lead to reduced autoimmunity in an MS model,” she said.
Other elements and stages of the research, which was published in PLOS Biology in 2023, showed increased apoptosis of CD4-positive immune cells in AHR-deficient mice and the ability of oral taurocholic acid — a bile acid that was especially high in mice without AHR — to reduce the severity of EAE, Merchak said.
Evidence for the role of gut and peripheral inflammation on neurodegeneration is building on numerous fronts, Merchak said. Unpublished research using spatial transcriptomics of colon biopsies from patients with inflammatory bowel disease (IBD), patients with Parkinson’s disease (PD), and neurologically healthy control individuals, for instance, showed similar cell communication patterns in patients with IBD or PD (and no history of IBD) compared with healthy control individuals.
And in research using a single-cell genomics approach and a mouse model of lipopolysaccharide (LPS)-induced system neuroinflammation, microglia were found to preferentially communicate with peripheral myeloid cells rather than other microglia after peripheral LPS exposure.
“In saline-treated mice, the microglia are talking primarily to microglia, but in LPS-treated mice, microglia spend more time communicating with monocytes and T cells,” Merchak explained. “We see communication going from inside the brain to cells coming in from the periphery.”
In another experiment, 2 months of a high-fat, high-sugar diet in mice with an engineered predisposition to frontotemporal dementia led to significant upregulation of major histocompatibility complex class II (MHC II) expression on monocytes in the brain, she said, describing unpublished research. Because MHC II handles antigen presentation in the brain, the change signals increased central-peripheral immune crosstalk and increased brain inflammation.
State of Clinical Research
On the clinical side, Merchak said studies of gut microbiome-modulating therapies are currently not longitudinal enough to accurately study neurodegenerative diseases that may develop over decades. Still, her review of the literature — part of her 2024 article — suggests there is at least some preliminary clinical evidence for the use of probiotics/prebiotics/diet and fecal microbiota transplant (FMT) in several diseases.
Parkinson’s Disease: “There has been some evidence,” Merchak said at the meeting, “for the treatment [with probiotics, prebiotics and diet] of nonmotor symptoms — things like gastrointestinal distress and mood changes — but no real evidence that such treatments can help with the motor symptoms we see in Parkinson’s.”
Over 60 patients with PD have been treated with FMT, she said, with reduced GI distress and mixed results with motor symptoms.
Alzheimer’s and related dementias: “Diet shows promise for cognitive outcomes, but there hasn’t been much evidence for probiotics,” she said. Her review found 17 patients diagnosed with dementia who were treated with FMT, “and for many of them, maintenance of cognitive function was reported — so no further decline — which is excellent.”
Multiple Sclerosis: “We see higher quality-of-life measures in patients getting probiotics, prebiotics, and changes in diet,” Merchak said. “Again, most of this [relates to] mood and digestion, but some studies show a slowing of neurological damage as measured by MRI.”
There are reports of 15 patients treated with FMT, and “three of these document full functional recovery,” she said, noting that longer follow-up is necessary as MS is characterized by relapsed and periods of recovery.
Merchak reported no financial disclosures.
Source link : https://www.medscape.com/viewarticle/gut-microbiome-likely-influences-neurodegenerative-disorders-2025a10007wv?src=rss
Author :
Publish date : 2025-04-02 12:45:00
Copyright for syndicated content belongs to the linked Source.