As a hematologist and researcher at Duke University, Durham, North Carolina, Lindsay Rein, MD, has taken opportunities to dive deeply into the study of cancer at the cellular level, as well as to participate in cutting-edge clinical trials of experimental medicines.
Yet, in a surprising way, her medical career resembles that of her mother, who worked as a primary care physician while raising Rein and her brother in North Dakota in the 1990s.
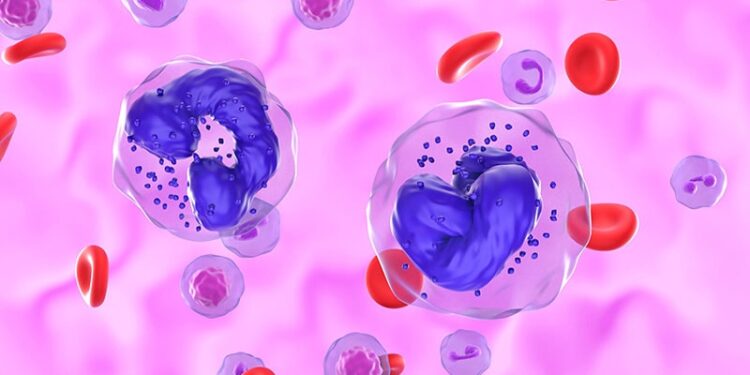
Advances in Rein’s specialty, the field of myeloproliferative neoplasms (MPNs), including chronic myeloid leukemia (CML), have allowed many patients to live for years with treatment.

“I’m treating a specialized group of diseases, but I’m also getting to know the patients and who they are as people, learning about their families,” Rein told Medscape Medical News. “That’s really fulfilling, to have these types of relationships with patients. It’s not the same as my mom did but kind of a similar principle.”
While the progress in CML may be best known there’s also been notable progress in other MPNS, she said.
For example, only a few years ago, there was little to offer patients with indolent systemic mastocytosis beyond therapies for symptoms. But now there are multiple agents that are in trials and in various stages of development with multiple mechanisms of action, Rein said.
“The research in this field has just exploded over the past several years,” she said.
Advances in molecular testing have set the stage for improved outcomes for people with MPNs, she said.
“That has really allowed us to understand the biology of these diseases better,” Rein said. “There’s been a lot more development of drugs that target specific pathways.”
There’s been a particularly remarkable change in CML treatment in recent decades due to the emergence of Bruton’s tyrosine kinase inhibitors (BTKis).
Consider that when Rein graduated from University of North Dakota, School of Medicine and Health Sciences, Grand Forks, North Dakota, in 2008, researchers were gaining a better understanding of the potential of the first BTKi used in CML, imatinib (Gleevec) and second-generation options for CML were starting to emerge.
The US Food and Drug Administration first granted an accelerated approval for imatinib in 2001, clearing it for use in CML during the blast crisis, accelerated phase or in chronic phase after failure of interferon-alpha therapy. Evidence soon allowed for approval of the drug’s use in other indications, including treating newly diagnosed adults with Philadelphia chromosome positive CML. Approvals for dasatinib (Sprycel) and nilotinib (Tasigna) came within a few years.
“I graduated right around the time when multiple options were being approved and when we could start tailoring therapy choices to individual patients,” Rein.
Other CML treatments followed: Asciminib (Scemblix), bosutinib (Bosulif), and ponatinib (Iclusig).
From 2011 to 2014, Rein did a hematology and medical oncology fellowship at Duke University Medical Center. Louis F. Diehl, MD, was among the staff physicians with whom she trained. He recalled for Medscape Medical News how Rein dove into MPNs.
“They were a special category, because they didn’t really belong to anybody before Lindsay came along in our division. We all did them, and some of us had investigative experience in some of those diseases, but there was nobody who said, “‘This is my class of disease,’” Diel noted.
“Lindsay took that on, and she has built that,” he added.
Diehl said he’s been in the fortunate position now of sometimes seeking help from a physician he helped train.
“It’s a wonderful thing, if you are a teacher or a mentor, to see that your mentee has surpassed you, and Lindsay has done that,” Diehl said.
He will now seek her opinion when deciding on treatments.
“The patients that we often get are patients where there is no textbook answer. You can’t say, ‘Put all these characteristics in, and this is the answer,’“ Diehl said. “We have to get it from somebody who can analyze various parts of the literature and say, ‘This is the best choice for the patient,’ and Lindsay has that kind of skill.”
Diehl said he sometimes sees patients who were treated earlier by Rein. Her compassion and ability to explain complex medical conditions makes her a favorite of patients, he said.
“She can translate it into language that everybody understands, and that people get the idea after talking to Lindsay that she is sincere and that she is telling them the truth, and she has their best interests at heart,” Diehl said.
“When you combine analytical ability, knowledge and the ability to communicate that as well as you’re communicating empathy and compassion, you’re one heck of a bedside doctor,” Diehl said. “And Lindsay is that.”
Rein has maintained an interest in basic science while also participating as an investigator for trials of newer drugs. She has studied whether multifunctional adapter proteins known as beta-arrestins (βarrs) could be targets for future drug discovery.
This work also feeds into her clinical practice.
“Spending some time in basic science teaches you how to create a hypothesis, how to ask questions,” Rein said. “Part of medicine is knowing what questions to ask, what the right questions are, how to ask the questions.
Rein and her husband, a gastroenterologist, both trained at Duke and have decided to stay in the area to raise their two children aged 6 and 8 years.
“What we’ve always been drawn to, and what’s always kept us here, is just the fact that it’s such a nice place to live” with many art and cultural options, Rein said. “We love that it’s close to the beach and close to the mountains, and you can get to most places relatively easily. We’ve just never, never found a place that we would rather be.”
Rein said travel is important to her family. So far, she has taken her children on trips that include skiing vacations as well as visits to Switzerland and Croatia. Going abroad gives the family a chance to try new foods and experience other cultures.
“I love that I can show my kids just a different way to think about things,” she said.
Rein sees parallels between her travels and her works with people who have MPNs.
“I only see people with a handful of diseases,” she said. “But what I find so fascinating is that every patient truly is different, right? So, they have their own unique experience with these diseases, their own unique presentation. Everybody tolerates the therapies differently. Everybody requires a different therapy.”
Kerry Dooley Young is a journalist who reported on medical research and health policy for more than 25 years. In addition to frequently appearing in Medscape Medical News, her work has been published by Bloomberg, CQ Roll Call, STAT and the Washington Post. blished by Bloomberg, CQ Roll Call, STAT and the Washington Post.
Source link : https://www.medscape.com/viewarticle/hematologist-dives-deep-mpn-research-explains-it-clearly-2025a10006xn?src=rss
Author :
Publish date : 2025-03-24 11:11:00
Copyright for syndicated content belongs to the linked Source.