Intraoperative frozen section histology (IFSH) demonstrates high diagnostic accuracy for individual surgical margins in human papillomavirus (HPV)-related oropharyngeal squamous cell carcinoma (OPSCC), but it may fall short in predicting final surgical margin status, according to the authors of new research.
Despite the limitations of IFSH, it remains a key tool for guiding intraoperative re-resection and improving outcomes reported lead author Salma Ramadan, MD, of Washington University School of Medicine in St. Louis, Missouri, and colleagues.
Why Was This Study Conducted?
“We were interested in how margins may or may not be useful in the management of HPV-related OPSCC ,” principal investigator Sidharth V. Puram, MD, PhD, of Washington University School of Medicine in St. Louis, said in an interview. “Evaluating the accuracy of IFSH can be helpful in providing guidance to surgeons on how best to use these approaches intra-op.”
The investigators noted that frozen section evaluation is known for high diagnostic accuracy; however, intraoperative techniques for head and neck squamous cell carcinoma have limited evidence.
“To our knowledge, no large-scale studies have investigated the use of IFSH in assessing final surgical margin status in HPV-related OPSCC, particularly in the context of contemporary transoral surgical approaches,” they wrote in JAMA Otolaryngology-Head Neck Surgery. “Given the favorable overall prognosis of HPV-related OPSCC and the morbidity of trimodal adjuvant therapy associated with positive surgical margins, large-scale studies on the use of frozen sections in HPV-related OPSCC are imperative.”
How Did the Study Evaluate the Reliability of IFSH for HPV-related OPSCC?
This study included 254 patients diagnosed with HPV-related OPSCC who underwent transoral surgery between 2015 and 2021. Patients were selected based on the availability of complete data for intraoperative and final surgical margin status. Cases comprised a range of tumor subsites, including both tonsil primaries and base-of-tongue (BOT) primaries, to evaluate the performance of IFSH across different anatomical areas.
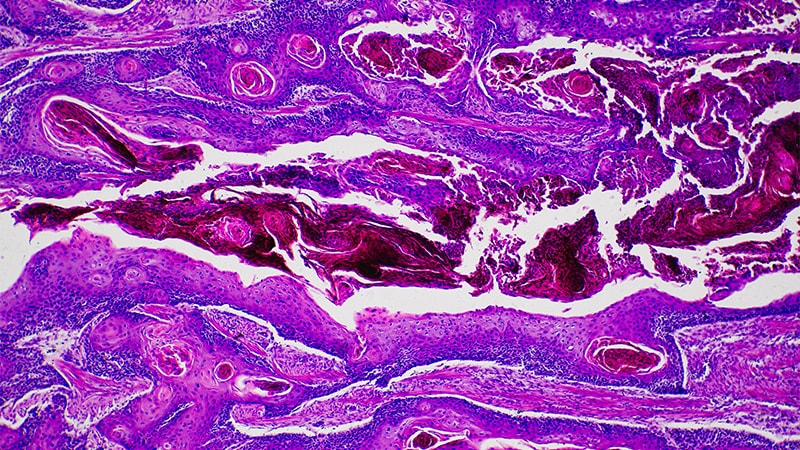
The investigators systematically examined 1482 surgical margins using IFSH to assess its accuracy in detecting positive and negative individual margins. These intraoperative results were compared with final tumor specimen histopathology (FTSH; ie, main specimen margin status) and the final surgical margin status, which was determined postoperatively using permanent histopathology.
The primary goal was to evaluate how effectively IFSH could guide surgical decisions and ensure optimal oncologic outcomes.
What Were the Key Findings?
IFSH exhibited high diagnostic accuracy for individual margins, with an overall accuracy of 97.1%, specificity of 99.1%, and a negative predictive value of 97.8%. These metrics confirm the reliability of IFSH in identifying negative margins intraoperatively, giving surgeons confidence when margins are deemed clear of disease.
In contrast, the sensitivity of IFSH for predicting final surgical margin status was low, at 21.7%. This indicates that while IFSH is effective for ruling out residual disease, it misses a substantial number of positive margins, with 7.1% of patients having at least one intraoperatively undetected positive margin.
Among 230 patients with negative final surgical margins, 105 (45.7%) had negative FTSH results and negative separately submitted margins, while 124 (53.9%) had positive FTSH results. Of those with positive FTSH, 56 initially had negative separately submitted margins and 68 had initially positive margins that were cleared through intraoperative re-resection. One tumor specimen could not be assessed directly but was considered negative due to all margins submitted being negative.
Positive final surgical margin status was significantly associated with worse disease-specific survival (hazard ratio [HR], 3.26; 95% CI, 1.05-10.13) and increased local and regional recurrence (HR, 5.02; 95% CI, 1.25-20.19) compared with negative status. While positive FTSH also trended toward worse survival (HR, 2.28; 95% CI, 0.73-7.07) and higher recurrence (HR, 2.57; 95% CI, 0.53-12.39), the wide confidence intervals limit the significance of these findings.
Although multivariable analysis was not feasible due to the low number of events (mortality and recurrence), positive surgical margin status remained significantly associated with worse survival and recurrence in early-stage (T1/T2) disease, independent of other pathological factors such as T stage, overall stage, and subsite, suggesting that positive surgical margins are an independent prognostic factor in this setting.
“It is well established that positive margins adversely affect outcomes and require adjuvant therapy, so this part was expected,” Puram noted.
Which Cases Were Most Challenging, How Might Challenges Be Overcome?
The study identified specific challenges in the assessment of BOT tumors and deep margins.
These cases were particularly prone to errors, with IFSH demonstrating a sensitivity of only 63.2% for deep margins compared to 77.1% for radial margins. For BOT tumors, the sensitivity dropped further, with IFSH identifying only 7.7% of positive margins intraoperatively, as opposed to 40.0% for tonsil primaries.
Sampling errors, such as missing the true positive areas or sectioning non-tumor regions, accounted for most of these inaccuracies. BOT tumors also presented unique anatomical hurdles, including their proximity to critical structures and increased risk for tissue retraction, which obscured tumor margins.
“In the future, intraoperative technologies such as ultrasound and other imaging-based modalities may be helpful in these contexts,” Puram said.
Emerging techniques like high-resolution intraoperative imaging could improve the accuracy of IFSH in challenging cases, offering surgeons a clearer view of complex tumor sites, the investigators explained. Adopting specimen-driven approaches — such as perpendicular margin sampling — could also enhance the accuracy of deep margin evaluation by ensuring comprehensive coverage of the resected tissue.
What Were the Study Limitations?
According to the investigators, the study’s retrospective design limited its ability to directly compare IFSH with a true specimen-based approach involving perpendicular margin sampling.
The analysis was further constrained by the low prevalence of positive margins, resulting in wide confidence intervals for positive predictive values.
Multivariate survival analysis could not be performed due to the small number of deaths and recurrences in the cohort.
In addition, generalizability is limited by the predominantly White patient population.
Although this research is the first to evaluate IFSH in HPV-related OPSCC treated with transoral surgery, larger, prospective studies across multiple institutions are needed to confirm these findings, the investigators noted.
How Should IFSH Change Clinical Decision-Making?
Despite the potential shortcomings of IFSH, the investigators supported its continued use.
“IFSH remains critical for optimizing oncologic outcomes in HPV-related OPSCC that is treated with transoral surgery,” they wrote.
Puram suggested that IFSH is part of a broader strategy that depends on close collaboration between colleagues.
“Our findings suggest that IFSH may be helpful in HPV+ OPSCC,” Puram said, “Most important though is the discussion between pathologist and surgeon to guide the final tumor margin status.”
Study co-author Ryan Jackson reported honoraria from Intuitive Surgical outside the submitted work. No other disclosures were reported.
Source link : https://www.medscape.com/viewarticle/how-reliable-intraoperative-frozen-section-histology-hpv-2025a10001rh?src=rss
Author :
Publish date : 2025-01-24 06:21:08
Copyright for syndicated content belongs to the linked Source.