ORLANDO, Fla. — Of the 12 biologics in four drug classes approved for treating psoriasis in the United States, interleukin 23 (IL-23) inhibitors might be exceptional, particularly if used early and in relatively high doses, according to two sets of research.
“There are now a lot of clinicians and researchers in psoriasis who believe that IL-23 inhibitors are unique relative to other biologics,” explained Anthony P. Fernandez, MD, said at the American Academy of Dermatology (AAD) 2025 Annual Meeting.
Specifically, based on its mechanism, “IL-23 is viewed by some as the overarching master cytokine in the psoriasis pathway,” said Fernandez, clinical assistant professor in the Department of Dermatology, Cleveland Clinic, Cleveland.
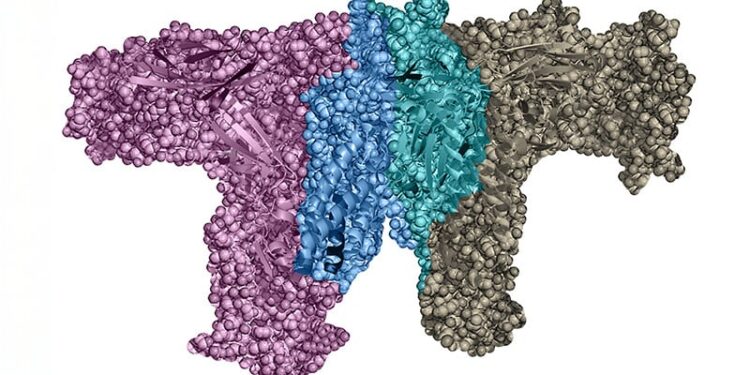
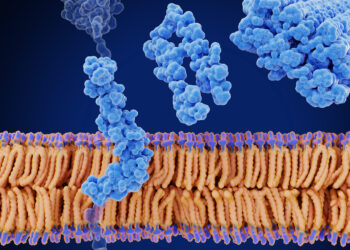
There are several reasons. One is that IL-23 is activated relatively upstream in the inflammatory cascade, so that blockade of this cytokine prevents expression of multiple downstream pro-inflammatory cytokines, such as IL-17A and IL-22.
IL-23 Drives T-Cell Activation Relevant to Psoriasis
But, perhaps more importantly, Fernandez said that IL-23 appears to be necessary for the survival of TRM17 memory cells. This is important because these long-lived memory cells preserve the information responsible for reactivating psoriasis when therapy is stopped, according to Fernandez.
Ultimately, these memory cells explain why psoriasis is a chronic recurring disease and why it usually recurs in the same location, he said.
Memory cells accumulate in the skin of patients with psoriasis over time. Based on their dependence on IL-23, the theory that early use of high-dose IL-23 inhibitors might “induce long-term remissions or even cure” was recently tested in a prospective phase 2 trial, Fernandez noted.
Although not yet published. Fernandez said the results are consistent with this hypothesis.
In this uncontrolled study, patients with severe psoriasis (involved body surface area over 10%) were enrolled and treated with the IL-23 inhibitor risankizumab. Rather than the standard dose, patients received either 300 mg or 600 mg, which are twice and four times greater, respectively. Doses were administered at weeks 0, 4, and 16. After the third dose, all therapy was stopped.
“No other medicine was prescribed, not even topicals, until the end of the study at 52 weeks,” said Fernandez. Disease activity was followed with Psoriasis Area and Severity Index (PASI) scores.
Pooling the data from the two arms, “60% of patients had maintained a PASI 90 response at week 52 despite not having had any medication for psoriasis since week 16,” Fernandez said.
“Forty percent were completely cleared,” he added, noting that the theory of benefit from blocking TRM17 memory cells was outlined in a 2022 editorial by the principle investigator Andrew Blauvelt, MD. In the Journal of Psoriasis and Psoriatic Arthritis editorial, Blauvelt, a practicing dermatologist and president of the Oregon Medical Research Center, Portland, Oregon, predicted that a relatively short course of high doses of IL-23 inhibitors would be accompanied by an extended period or remission accompanied by a reduction in the TRM17 memory cells, and this was exactly what was observed.
Memory T Cells Reduced by IL-23 Inhibitors
“When they looked at the lesional skin, there was in fact a significant reduction in the number of pathogenic memory T cells at week 52 compared to week 0,” Fernandez reported.
On the basis of these results, he predicted that more studies like this will come. If they produce similar results “the way that we administer IL-23 inhibitors to our patients may change,” he said.
The early use of IL-23 inhibitors in aggressive doses might also change for another reason. Several observational studies with biologics other than IL-23 inhibitors have suggested that it might be possible to prevent patients with plaque psoriasis from progressing to psoriatic arthritis (PsA). Now, a phase 4 study with an IL-23 inhibitors is testing the hypothesis with a prospective design.
In this ongoing randomized, double-blind study called PAMPA (a description was published in 2022 in BMJ Open), patients with psoriasis are being randomly assigned to the IL-23 inhibitors guselkumab or placebo groups after an initial screening period. The coprimary endpoints are changes from baseline in an ultrasound musculoskeletal score at week 24 and the difference in the proportion of patients with PsA at 96 weeks.
Data are not yet mature, but this study, if positive, could also change the status of IL-23 inhibitors relative to other biologics in this disease. Indeed, Fernandez pointed out that long remissions and protection against PsA in patients with psoriasis are both major unmet needs.
One of the most prolific trialists in psoriasis, Mark Lebwohl, MD, chairman emeritus of the Department of Dermatology at the Icahn School of Medicine at Mount Sinai, New York City, New York, was asked to comment.
Based on his own experience and other data, “IL-23 blockade does indeed result in long remissions of psoriasis, supporting ernandez’s view,” he said.
Although these observations validate the effort to test new strategies for enhancing prolonged remissions with IL-23 inhibitors, he warned that validating a role for IL-23 inhibitors in preventing PsA is likely to prove “more complicated.”
“Studies showing that IL-23 blockade prevents arthritis are not as straightforward because IL-17 blockade is more effective for PsA,” he said. As a result, “many patients with joint pain are put on IL-17 blockers or TNF [tumor necrosis factor] blockers, not only IL-23 blockers, thus leading to challenging bias.”
Fernandez reported financial relationships with AbbVie, AstraZeneca, Biogen, Bristol Myers Squibb, Castle Biosciences, Kyowa Kirin, Mallinckrodt, Novartis, Pfizer, Priovant, and UCB. Lebwohl reported financial relationships with more than 30 pharmaceutical companies, including multiple companies that manufacture IL-23 inhibitors and other biologics.
Source link : https://www.medscape.com/viewarticle/anti-il-23-therapy-might-emerge-best-biologic-psoriasis-if-2025a10006of?src=rss
Author :
Publish date : 2025-03-20 13:13:00
Copyright for syndicated content belongs to the linked Source.