Every week, 4000 young cisgender women aged 15-24 years contract HIV globally, according to 2023 data. Infections in this age group accounted for 44% of the new global infections that year, highlighting the vulnerability of this population to AIDS.
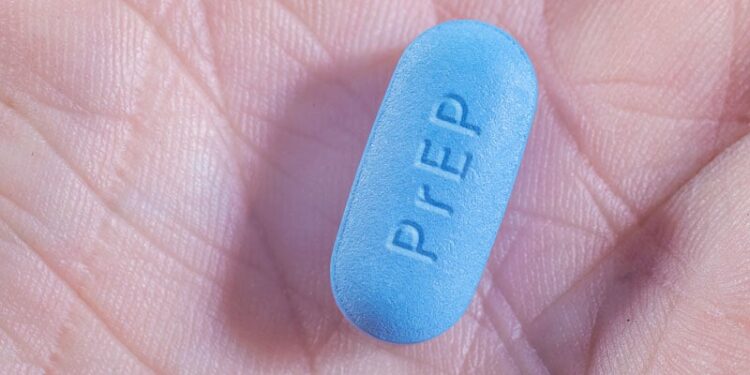
Despite these alarming figures, awareness of and access to preventive measures, such as pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP), remain limited among women and healthcare professionals.
This situation reflects a global trend in Brazil. According to data from the HIV and AIDS Epidemiological Bulletin, published in December 2024 by the Ministry of Health, there were 125,753 reported cases of HIV among young people aged 15-24 years between 2013 and 2023, representing 23.2% of the national total. Of these patients, 24.8% were men and 19.4% were women, highlighting the urgent need for public policies on prevention, early diagnosis, and accessible treatment for this age group.
Another concern is the increase in HIV infections among women over 50 years of age. In this age group, the proportion of women increased from 12.8% in 2013 to 21.1% in 2023, whereas the proportion of men increased from 9% to 12%. These findings indicate the need for strategies that address the specific needs of women at different stages of life, including prophylaxis, early detection, and prevention of HIV transmission in infants.
Invisible Barriers
Despite the significant risks that women face, numerous interconnected barriers hinder the widespread adoption of PrEP and PEP. One major challenge is the misperception of personal risk.
A study conducted in the United States found that only 37.5% of participants initially expressed interest in PrEP. After educational sessions on medication, this number dropped to 2.8%, revealing that underestimating risk is a critical obstacle to adopting preventive measures.
Lack of awareness regarding PrEP is also prevalent. A systematic review conducted in the United States found that only one third of the women were aware of prophylaxis, although many expressed interest when informed. This lack of awareness is worsened by the absence of targeted educational campaigns and the stigma associated with medication. In a 2017 survey of 597 women at family planning clinics, 37% associated PrEP use with promiscuity, and 32% believed it was a sign of HIV status. These misconceptions discourage open discussions with healthcare providers and contribute to the spread of misinformation.
Another significant challenge is the lack of proper guidance from healthcare professionals. Many providers are hesitant to prescribe PrEP because of inadequate training or unfamiliarity with guidelines. Furthermore, in another US study, negative interactions with healthcare providers were identified as a major reason for discontinuing prophylaxis. This highlights the need for ongoing professional education and more sensitive and consistent follow-up for patients.
Socioeconomic and structural barriers further affect adherence to PrEP. Other factors include high costs, a lack of insurance coverage, and limited access to medical services. A qualitative study conducted in South Africa, including women with higher education, found that social judgment and relationship dynamics often hinder access to PrEP. These challenges are not confined to one region and require an integrated, sensitive approach to promote prevention and care.
Prophylaxis Options
The development of prophylactic options offers hope for tackling the epidemic more effectively. In addition to the traditional oral routes, new alternatives are emerging to improve adherence and reduce stigma.
A review published in Therapeutic Advances in Infectious Disease discussed new approaches to HIV prophylaxis for women, marking a significant step in a previously neglected field. These advancements include technological and pharmaceutical innovations aimed at increasing adherence; improving efficacy; and overcoming social, cultural, and logistical barriers.
One of the most promising options is long-acting injectable cabotegravir, an antiretroviral medication that has proven to be superior to the oral combination of tenofovir disoproxil fumarate and emtricitabine (TDF/FTC). Clinical studies have shown that cabotegravir administered every 2 months significantly lowers the risk for HIV infection. This option provides greater discretion and convenience, which are essential for women who face challenges with the use of daily pills because of stigma and complex social dynamics.
Another innovative alternative is the dapivirine vaginal ring, which has been approved by the World Health Organization. The monthly use of this device is a highly effective preventive tool, particularly for individuals with greater social vulnerability or limited access to medical care. Studies have shown that the ring can reduce HIV incidence by up to 62% and is well tolerated and widely accepted by patients.
Subdermal implants have also been explored for sustained release of antiretrovirals. These devices have the potential to provide continuous protection for several months, minimizing the need for frequent medical follow-ups and increasing women’s autonomy over their sexual health.
Additionally, vaginal films containing nanomicelles of bictegravir are currently undergoing clinical trials as a practical and discreet preventive option. Although still in the early stages, these advancements have addressed the specific needs of women.
The Brazilian Ministry of Health has adopted established strategies for PrEP and PEP for HIV, as described in the 2022 Clinical Protocol and Therapeutic Guidelines.
For PrEP, the combination of TDF/FTC is recommended as a daily pill for men and women at high risk for HIV infection. For PEP, a 28-day regimen with three antiretrovirals (tenofovir, lamivudine, and dolutegravir) is recommended after high-risk exposure.
Prophylaxis for Special Populations
Women vulnerable to HIV face diverse challenges, including social, cultural, and structural barriers that hinder their access and adherence to prophylaxis.
The review published in Therapeutic Advances in Infectious Diseases focused on pregnant and postpartum women, victims of sexual violence, and adolescents.
Pregnant or postpartum women must protect their health while preventing the transmission of HIV to their infants. Studies have shown that TDF/FTC prophylaxis is safe and effective; however, stigma and inconsistent guidelines in some regions complicate this process.
Similarly, adolescents and young women often struggle with gender norms and social expectations that limit their ability to seek prevention because of misinformation and stigma. In both cases, fear of judgment and a lack of community support were common barriers.
Victims of sexual violence often face power dynamics that restrict their access to preventive care. Fear of disclosing PrEP use to partners and distrust in healthcare systems reflect the challenges faced by adolescents and young women in patriarchal environments. To overcome these obstacles, it is crucial to build support networks and foster trust between patients and healthcare providers.
Despite their different experiences, these populations share a common need for sensitive and inclusive approaches that recognize their specific needs and address their common needs. By integrating PrEP services into reproductive health clinics to launch educational campaigns, each action can contribute to making prophylaxis accessible and effective.
A Possible Future
Despite barriers to PrEP and PEP implementation among women, success stories from around the world show that these challenges can be overcome. Creative solutions, inclusive approaches, and collaborative efforts can turn HIV prevention into a universal resource that can protect women, regardless of their circumstances.
A study in Brazil found that younger age and lack of social support were significant factors for discontinuation from follow-up after PEP. This reality, far from being exclusive to Brazil, reflects the challenges faced globally where misinformation, stigma, and structural barriers often impede access to prophylaxis. Integrating PrEP and PEP services with reproductive health and primary care programs has proven effective in reducing discontinuation rates and improving patient outcomes.
A program in Kolkata, India, incorporated PrEP into community initiatives for women sex workers, demonstrating the transformative power of community engagement and peer support on treatment adherence. In Brazil, exploring similar strategies adapted to local cultural and structural realities could help mitigate stigma and expand access, especially in remote areas, where inequalities are most evident.
Furthermore, digital technology has emerged as an indispensable tool. Telemedicine, mobile apps, and electronic health records help eliminate geographical barriers, improve communication between patients and healthcare professionals, and strengthen monitoring and adherence to treatment. These tools modernize care and ensure that prophylaxis reaches those who need it the most.
The successful implementation of HIV prophylaxis involves more than just pharmacological advancements. This requires a comprehensive approach that combines scientific innovation, empathy, and inclusive public policy. With coordinated efforts tailored to specific needs, it is possible to ensure that no woman is left behind in the fight against HIV. Transforming prevention into an accessible right guarantees dignity, health, and opportunities for all.
This story was translated from Medscape’s Portuguese editionusing several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Source link : https://www.medscape.com/viewarticle/innovations-hiv-care-women-worldwide-2025a10000s0?src=rss
Author :
Publish date : 2025-01-14 05:12:51
Copyright for syndicated content belongs to the linked Source.