TOPLINE:
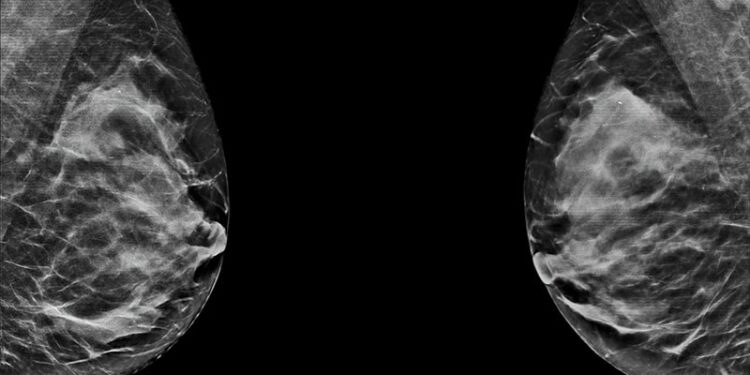
Compared with digital mammography, digital breast tomosynthesis (also known as 3D mammography) improved specificity and reduced recall rates in women with a family history of breast cancer, particularly in those with one first-degree relative, a new analysis revealed. Tomosynthesis also detected a higher proportion of early-stage invasive cancers with favorable prognostic features and reduced rates of advanced cancer in women with extremely dense breasts, which suggests that more aggressive tumors are diagnosed at an earlier stage, the researchers explained.
METHODOLOGY:
- Women with a family history of breast cancer are at an increased risk for the disease and are more likely to have dense breast tissue, which can make it harder to identify cancers on standard mammography. While tomosynthesis can detect more cancers in both fatty and dense breasts, research comparing tomosynthesis and digital mammography in women with a family history of breast cancer has been limited.
- A comparative cohort study examined 208,945 women with a family history of breast cancer who underwent 502,357 screening examinations from 2011 to 2018, including 121,698 tomosynthesis (median age, 58 years) and 380,561 digital mammography (median age, 57 years) examinations.
- Overall, 4.4% of examinations were performed in Asian or Pacific Islander women, 13.3% in Black women, 4.4% in Hispanic or Latina women, 75.1% in White women, and 2.8% in women of unknown, or other, race.
- Family history was categorized into three groups: At least two first-degree relatives, one first-degree relative, or only second-degree relatives with breast cancer.
- Researchers assessed absolute risk differences (ARDs) between tomosynthesis and digital mammography for recall rate, cancer detection rate, advanced cancer rate, biopsy rate, positive predictive value, and specificity.
TAKEAWAY:
- Tomosynthesis was associated with a lower recall rate (ARD, −1.51%) and higher specificity (ARD, 1.56%) than digital mammography. These differences were more pronounced in women with one first-degree relative with breast cancer (ARDs, −1.72% and 1.75%, respectively).
- Among women with only second-degree relatives with breast cancer, tomosynthesis was associated with significantly higher biopsy rates (ARD, 0.39%) and false positive biopsy recommendation rates (ARD, 0.28%) than digital mammography.
- Among women with scattered fibroglandular densities, tomosynthesis reduced the recall rates (ARD, −1.90%) and improved specificity (ARD, 1.93%) compared with digital mammography. And among women with extremely dense breasts, tomosynthesis increased biopsy rates (ARD, 0.48%) but reduced advanced cancer rate (ARD, −0.61 per 1000 examinations).
- Tomosynthesis also reduced recall rates in women younger than 40 years (ARD, −4.65%) and those aged 60-69 years (ARD, −1.60%) while improving specificity. Tomosynthesis detected a higher proportion of early-stage invasive cancers with favorable prognostic characteristics than digital mammography.
IN PRACTICE:
“Our study provides new evidence to guide the use of [digital breast tomosynthesis] in screening women with a family history of breast cancer, suggesting that [digital breast tomosynthesis] may be used more generally in this population or selectively based on breast cancer family history category and for extremely dense breasts,” the authors wrote.
SOURCE:
This study, led by Tong Li, PhD, The Daffodil Centre, The University of Sydney, Sydney, Australia, was published online in JAMA Oncology.
LIMITATIONS:
A small number of interval and advanced cancers could have affected the statistical power to detect smaller differences. Analysis was restricted to women with complete 1-year follow-up data in the cancer registry, which limited subgroup analysis. Additionally, the study population was predominantly non-Hispanic White women, which limited generalizability of findings.
DISCLOSURES:
This study was supported by grants from the Cancer Institute New South Wales and National Health and Medical Research Council and the Breast Cancer Surveillance Consortium with funding from the National Cancer Institute. Several authors reported receiving grants from one of these organizations during the conduct of the study and/or outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Source link : https://www.medscape.com/viewarticle/mammography-better-women-family-history-breast-cancer-2025a1000e0o?src=rss
Author :
Publish date : 2025-05-29 06:24:00
Copyright for syndicated content belongs to the linked Source.