TOPLINE:
Different Kirsten rat sarcoma virus (KRAS) mutations in pancreatic ductal adenocarcinoma show varying treatment responses, with G12D and G12V mutations linked to worse outcomes compared with wild type.
METHODOLOGY:
- Researchers conducted a retrospective cohort study analyzing deidentified clinical data from 2433 patients with metastatic pancreatic ductal adenocarcinoma (PDAC), diagnosed between February 2010 and September 2022.
- They assessed the association of KRAS mutations in metastatic PDAC with the clinical outcomes and responses to first-line chemotherapy regimens.
- Data originated from approximately 280 US cancer clinics, encompassing about 800 sites of care, with comprehensive genomic profiling performed on all patients.
- Analysis focused on median overall survival (OS) and time to next treatment (TTNT) across different KRAS mutation groups, using multivariate Cox proportional hazards models.
TAKEAWAY:
- Patients with KRAS G12D and G12V mutations showed significantly higher risk for disease progression (hazard ratio [HR], 1.15; 95% CI, 1.04-1.29; P = .009) and (HR, 1.16; 95% CI, 1.04-1.30; P = .01), respectively, compared with KRAS wild type.
- KRAS G12R mutations were associated with the longest median OS at 13.2 months (95% CI, 10.6-15.2) and longest median TTNT at 6.0 months (95% CI, 5.2-6.6).
- FOLFIRINOX treatment demonstrated better outcomes than gemcitabine-based therapies across all patients, with lower risk for treatment progression (HR, 1.19; 95% CI, 1.09-1.29; P P
- Specifically, when FOLFIRINOX was used as first-line treatment in patients with KRAS G12D and G12V mutations, the therapy was associated with improved TTNT and OS vs gemcitabine with or without nab-paclitaxel.
IN PRACTICE:
“In its totality, these data set a benchmark for future studies on KRAS inhibitors for specific KRAS variants and highlights the groups for which treatment combinations may ultimately be necessary,” the authors concluded about the findings of their new research.
SOURCE:
The study was led by Carter Norton, Huntsman Cancer Institute in Salt Lake City, Utah. It was published online on January 7 in JAMA Network Open.
LIMITATIONS:
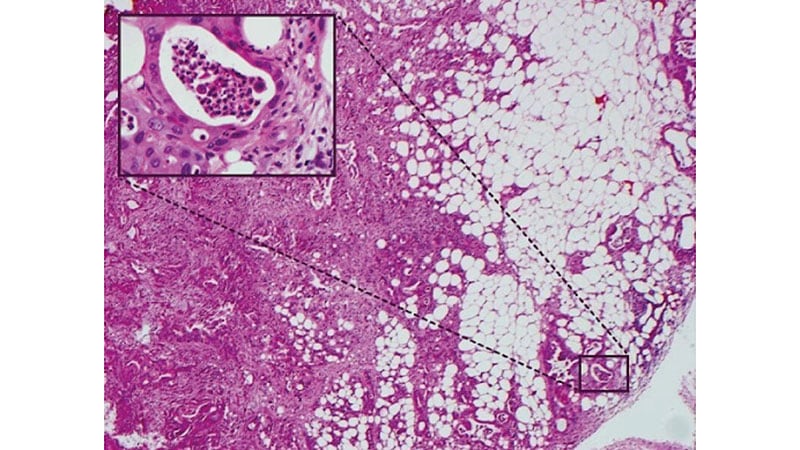
According to the authors, the study’s limitations include the heterogeneity of clinical data collected retrospectively, which is subject to residual confounding. The sample size was limited for certain mutational groups, particularly KRAS G12C, leading to limited statistical power. Additionally, the detection rate of genomic alterations by commercially available assays may be affected by the high stromal content and low cellularity characteristic of PDAC.
DISCLOSURES:
The study was supported by Cancer Center Support grant P30CA042014 from the National Institutes of Health. Heloisa P. Soares, MD, PhD, one of the study authors, disclosed receiving consulting fees from Ipsen, Exelixis Inc, BMS, Novartis AG, AstraZeneca, and TerSera Therapeutics LLC and symposium speaker fees from ITM Radiopharma outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Source link : https://www.medscape.com/viewarticle/kras-mutations-linked-varied-treatment-outcomes-metastatic-2025a10000fq?src=rss
Author :
Publish date : 2025-01-09 08:23:15
Copyright for syndicated content belongs to the linked Source.