[ad_1]
LOS ANGELES — Clinicians working in advanced heart failure vented their frustrations about the shrinking number of device therapies left from round after round of FDA recalls. Could a changed regulatory climate under the Trump administration bring about more treatment options?
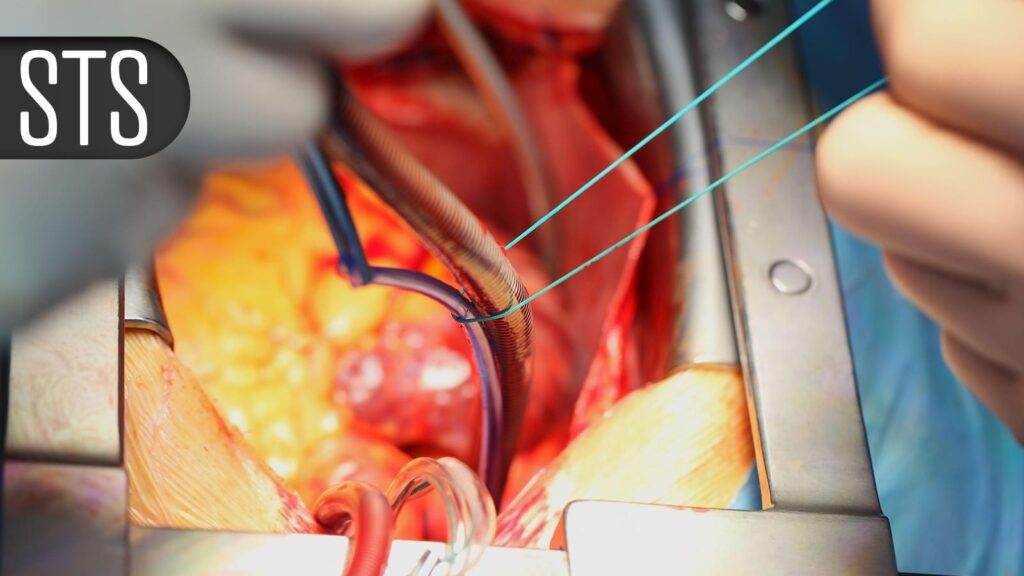
The question came up during an audience Q&A session at the Society of Thoracic Surgeons (STS) annual meeting. While panelists were generally hesitant to make predictions about politics, Richard Lee, MD, JD, MBA, of Augusta University Medical Center in Georgia, laid out how things could go two ways in the years ahead.
One is a push to move device development faster along in industry, with a higher tolerance for defects. On the other hand, the reduced government support for research funding, evident already, would suggest no economic support for medical device makers.
“I personally think it’s going to be both,” said Lee. “I could be wrong.”
A renewed appetite for innovation would bring some relief to the field of advanced heart failure in particular, which is now down to just one durable left ventricular assist device (LVAD) on the market, the HeartMate III. In 2021, the competing HeartWare ventricular assist device had been pulled for pump stop events, plus excess neurological events and mortality when compared with LVADs.
A recent study identified 157 cardiovascular devices recalled from 2013 to 2022. Recalls were commonly attributed to device design (31.4%), process control (16.1%), or component design or selection (7.3%).
At STS, physicians shared how they were navigating the various FDA recalls and the medicolegal implications of using devices under these recalls.
Courtney Maxey-Jones, MD, of CNY Medical Services in Baldwinsville, New York, recounted her experiences seeing device after device taken out of commission for various reasons when she could have still used them to save patient lives. In one instance, her hospital administrators had locked up all the Cardiohelp systems that were subject to a class I recall due to stiff hand cranks impeding an emergency drive.
Those were decisions made by “people who didn’t have to look at the patients that no longer had [the device] as an option,” Maxey-Jones lamented. “In order to be able to continue to provide high-level care to, frankly, the sickest of the sick patients, I’m not choosing a new prescription med. I’m deciding if I can give you mechanical circulatory support so that you don’t die in front of me.”
“If we’re going to continue to be the best advocates for our patients, we need to continue to insist on and invest in a diverse portfolio of mechanical support devices, which we can then match to our individual patient needs,” stressed Leora Yarboro, MD, of UVA Health in Charlottesville, Virginia.
“When something’s removed and not replaced with something that is also going to do the same thing for your patients, you really hope that you’re going to have some therapies for them. It’s our job … to make sure that patients who are supported with the device continue to be followed and supported as well, even if the device itself is no longer being manufactured,” she said.
So which devices are still okay to be used in clinical practice?
“Maybe we’re going to be sued for it, but I think it’s still reasonable to provide the best effort that you can … to save people’s lives with the tools that we have available,” said Yarboro.
“All technology has limitations, and it’s our shared responsibility to identify and report findings through our registry data … In this way, we can continue to be the best advocates for our patients, and remember that the goal behind reporting is not to have these life-saving devices be removed from the market, rather to ensure that the technology continues to evolve and to allow for informed decision-making by all,” she said.
Lee, a practicing lawyer, provided some reassuring data about the legalities of using medical devices under recall. In searching the national database, and consulting with lawyers who work with personal injury law, he could only identify two cases where a physician was named for failure to incorporate an action after receiving a recall notice — both got dismissed. “Right now, this is virgin territory,” he said.
What is more legally worrying is off-label use of drugs and devices, which he said he now avoids as much as he can.
Good communication with the patient and the patient’s family is key, according to Lee.
For example, the Impella 5.5 with SmartAssist is technically under class I recall and affected products are advised to be avoided unless no other product is available. As for Impella-assisted high-risk surgery, “I love it, and this is not an endorsement … I’m not going to stop doing it,” said Lee.
“I am not. I’m going to increase doing it, but now I’m going to tell every single patient ‘I’m doing this, they’re doing education for it, and you will have a risk … You can get a clot in the thing and it goes up to your head,'” he added.
If the patients say “no,” then he will back off on the procedure, he said.
Disclosures
Lee is a partner at Hochman and Lee, LLC.
Maxey-Jones had no disclosures.
Yarboro disclosed a prior speaker/honoraria relationship with Arthrex.
Please enable JavaScript to view the comments powered by Disqus.
[ad_2]
Source link : https://www.medpagetoday.com/meetingcoverage/sts/113964
Author :
Publish date : 2025-01-27 22:05:00
Copyright for syndicated content belongs to the linked Source.