Health reporter, BBC News
 Getty Images
Getty ImagesRepeated failures in how CTs, X-rays and other medical scans are being interpreted are leading to avoidable patient deaths and delays in diagnosing cancer, England’s health ombudsman has warned.
The most common problems include doctors failing to spot abnormalities, scans being delayed or not carried out, and results not being followed up properly.
The ombudsman has upheld or partially upheld 45 cases which include failures in medical imaging in the last four years, and says lessons must be learned to avoid the same mistakes again.
NHS England said staff work extremely hard to keep patients safe but acknowledged there was more to do to improve the “response to serious health issues”.
 Getty Images
Getty Images‘My dad’s note said he took his life because of the pain’
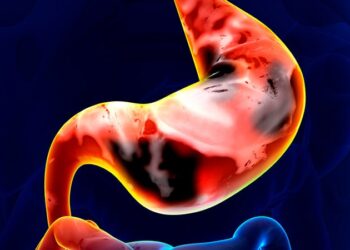
In one case, medical staff at Wexham Park Hospital in Slough repeatedly failed to diagnose an 82-year-old man with bowel cancer and left him suffering prolonged pain, according to the parliamentary and health service ombudsman (PHSO).
The man, from Buckinghamshire, went to A&E five times between August and October 2021.
A scan taken in August showed a lesion in the bowel.
However, clinicians reported no abnormalities, the investigation found, leading to a six-week delay in diagnosis and surgery.
The patient also had an X-ray in October that suggested an obstruction in his small bowel, but this X-ray was not reviewed and he was discharged and sent home.
Later that month the cancer was diagnosed and he had an operation to remove part of the bowel. The surgery uncovered another mass elsewhere in his body.
Just months later, the man took his life, leaving a note saying he could no longer deal with the pain.
The ombudsman, Rebecca Hilsenrath KC, said staff failed to manage his pain on five occasions.
Failings in his care “were probably contributory factors to the patient’s decision to end his life”, her report suggests.
The man’s daughter said: “I really tried to get the doctors to listen.
“I had a feeling something was wrong and I pleaded numerous times for them to keep him in the hospital, but they just kept discharging him and not doing anything to help him.”
A statement provided by the hospital trust says: “We are very sorry for our failing in care in this case and we have a further meeting with the patient’s family shortly to update them on the changes we have since made.
“This includes ensuring that older patients presenting with abdominal pain are appropriately reviewed.”
The trust has also agreed to pay the family £4,000, as recommended by PHSO.
‘My brother believed NHS was best place’
 Getty Images
Getty ImagesIn another investigation, the ombudsman found a cancerous tumour was incorrectly identified as benign (non-cancerous) – despite repeated scans suggesting otherwise.
The patient, a 54-year-old man, had his first scan in Tenerife, after becoming unwell on holiday.
His brother said: “When my brother collapsed in Tenerife, the hospital immediately identified the tumour for what it was [an aggressive brain tumour] and even offered to remove it.
“But my brother wanted to come home, he thought the best place for him to have the treatment was in the NHS.”
The man returned to Gillingham, where the local hospital carried out further scans identifying the tumour, and referred him to specialists at King’s College Hospital.
However, staff there “downgraded the diagnosis”, saying the tumour was not cancerous. The man was not offered chemotherapy or radiotherapy.
He died in hospital, a month after an operation to remove the tumour, which was confirmed to be cancerous.
If the cancer had been identified correctly, he could have had surgery months earlier and potentially the option of chemotherapy and radiotherapy, PHSO said.
While the survival rate for this cancer is poor, the ombudsman’s investigation suggests the man may have had a few extra months of life.
His brother said: “I wanted King’s College Hospital to acknowledge their mistakes so that I can stop picking at the scab of trying to understand what happened to him and remember my brother as he was when he was alive.”
In a statement, King’s College Hospital NHS Foundation Trust said: “We fully recognise that errors were made in this patient’s care, and we apologised to his family at the time of the incident.
“Learning from mistakes when they occur is crucial, and we have made a number of changes as a result of this case to improve the safety and effectiveness of the care our teams provide.”
The trust has agreed to pay the family £3,500.
‘Devastating consequences’
Ms Hilsenrath, whose team independently investigates complaints, said: “Each of the cases we have investigated and upheld represent a real person whose life has been impacted by failings in care.
“They are also all instances where the organisations involved failed to identify that anything had gone wrong”
The 2021 ombudsman report into medical imaging issues recommended system-wide improvements, but Ms Hilsenrath said while there had been some progress, she was still seeing instances where people’s care was “sub-optimal, often with devastating consequences”.
It is “critical” that action is taken to improve the digital infrastructure in the NHS and ensure people are diagnosed and treated swiftly, she added.
Dr Katharine Halliday, president of the Royal College of Radiologists, agreed digital infrastructure needed improvements.
“The ombudsman highlights some devastating failures in the NHS, and we must collectively learn from these experiences to drive meaningful change,” she said.
“However, it must also be recognised that these findings reflect a system that is overburdened and under-resourced.”
The college says it faces a 30% shortfall of clinical radiologists, which is projected to rise to 40% by 2028.
An NHS spokesperson said: “The NHS had delivered a record number of tests and checks in 2024, a fifth more than pre-pandemic but we know there is more to do to improve the recognition and response of serious health issues.”
A Department of Health and Social Care spokesperson said: “Our deepest sympathies are with all those who have been affected by the failings highlighted in this shocking report.”
The spokesperson added that they were opening more Community Diagnostic Centres (CDCs), and using new technology like AI so “all patients can receive world-class care”.
Changes were also being introduced in cancer care, the spokesperson said, which would see 100,000 more patients who are referred receiving a diagnosis within four weeks and up to 19,000 more people starting their treatment within two months each year.
Source link : https://www.bbc.com/news/articles/cdjykmlr2vwo
Author :
Publish date : 2025-03-21 02:21:00
Copyright for syndicated content belongs to the linked Source.