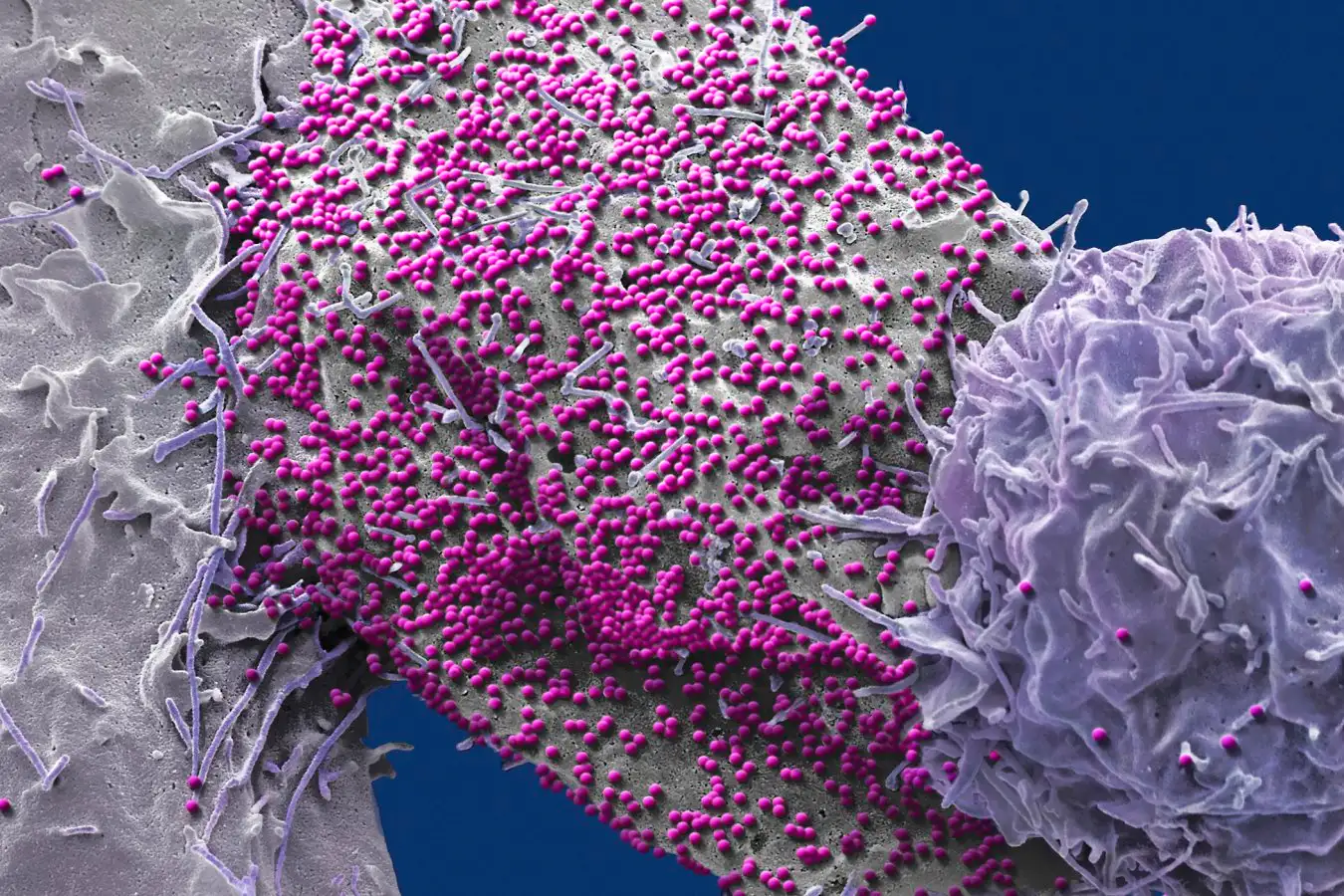
An HIV-infected human cell
STEVE GSCHMEISSNER/SCIENCE PHOTO LIBRARY
A man has become the seventh person to be left HIV-free after receiving a stem cell transplant to treat blood cancer. Significantly, he is also the second of the seven who received stem cells that were not actually resistant to the virus, strengthening the case that HIV-resistant cells may not be necessary for an HIV cure.
“Seeing that a cure is possible without this resistance gives us more options for curing HIV,” says Christian Gaebler at the Free University of Berlin.
Five people have previously become free of HIV after receiving stem cells from donors who carried a mutation in both copies of a gene encoding a protein called CCR5, which HIV uses to infect immune cells. This led scientists to conclude that having two copies of the mutation, which completely removes CCR5 from immune cells, was crucial for curing HIV. “The belief was that using these HIV-resistant stem cells was essential,” says Gaebler.
But last year a sixth person – known as the “Geneva patient” – was declared free of the virus for more than two years after receiving stem cells without the CCR5 mutation, suggesting CCR5 isn’t the whole story – although many scientists think the roughly two-year virus-free period isn’t quite long enough to show they were actually cured, says Gaebler.
The latest case strengthens the idea that the Geneva patient has been cured. It involves a man who, in October 2015, received stem cells to treat leukaemia, a type of blood cancer where immune cells grow uncontrollably. The man, who was aged 51 at the time, had HIV. During his treatment, he was given chemotherapy to destroy the vast majority of his immune cells, making room for the donor stem cells to produce a healthy immune system.
Ideally, the man would have received HIV-resistant stem cells, but these weren’t available, so doctors used cells that carried one typical and one mutated copy of the CCR5 gene. At the time, the man was taking a standard HIV therapy called antiretroviral therapy (ART), a combination of drugs that suppress the virus to undetectable levels, meaning it can’t be passed on to other people – and reducing the risk that the donor cells would be infected.
But about three years after the transplant, he chose to stop taking ART. “He felt that he’d waited some time after the stem cell transplant, he was in remission for the cancer, and he was always feeling that the transplant would work,” says Gaebler.
Shortly after, the team found no signs of the virus in blood samples from the man. He has since remained free of the virus for seven years and three months, enough for him to be considered “cured”. He has had no detectable HIV in his body for the second longest period of the seven people declared free of the virus – with the longest case being HIV-free for about 12 years. “It’s amazing that 10 years ago his chances of dying of cancer were extremely high and now he’s overcome this deadly diagnosis, a persistent viral infection and he’s not taking any medications – he’s healthy,” says Gaebler.
The discovery upends our understanding of what’s required for curing HIV via this approach. “We thought you needed to transplant from donors that lack CCR5 – it turns out that you don’t,” says Ravindra Gupta at the University of Cambridge, who wasn’t involved in the study.
Scientists have generally thought that such cures relied on any virus lurking in the recipient’s remaining immune cells – following chemotherapy – being unable to infect the donor cells, meaning it can’t replicate. “Essentially, the pool of host cells to infect runs dry,” says Gaebler.
But the latest case suggests that, instead, cures can be achieved as long as non-resistant donor cells are able to destroy any of the patient’s remaining original immune cells before the virus can spread to them, speculates Gaebler. Such immune reactions are often driven by differences in the proteins displayed on the two sets of cells. These make the donor cells recognise residual recipient cells as a threat to eliminate, says Gaebler.
The findings suggest that a wider pool of stem cell transplants than we thought – including those without two copies of the CCR5 mutation – could potentially cure HIV, says Gaebler.
But it is likely that many factors, such as the recipient’s and donor’s genetics, need to align in order for this to work, so that, for instance, the donor’s cells can rapidly destroy the recipient’s. What’s more, in the latest case, the man carried one copy of the CCR5 mutation, which could have altered how his immune cells were spread across the body in a way that made it easier to cure him of the virus, says Gaebler.
This means that most people receiving stem cell transplants for HIV and blood cancer should be offered HIV-resistant stem cells where possible, says Gaebler.
It’s also important to point out that cancer-free people with HIV won’t benefit from stem cell transplants, as it’s a very risky procedure that can lead to life-threatening infections, says Gaebler. Most people are better off taking ART – often in the form of daily pills – which is a much safer and convenient way to stop HIV from spreading, enabling people to enjoy long and healthy lives, he says. Moreover, a recently available drug called lenacapavir provides nearly complete protection against HIV with just two injections per year.
Nonetheless, efforts are being made to cure HIV by genetically editing immune cells, and prevent it using vaccines.
Topics:
Source link : https://www.newscientist.com/article/2506595-man-unexpectedly-cured-of-hiv-after-stem-cell-transplant/?utm_campaign=RSS%7CNSNS&utm_source=NSNS&utm_medium=RSS&utm_content=home
Author :
Publish date : 2025-12-01 16:00:00
Copyright for syndicated content belongs to the linked Source.