[ad_1]
A new trial of a minimally invasive surgical approach to removing the hematoma in patients with spontaneous intracerebral hemorrhage (ICH) has shown some encouraging results, despite a neutral primary endpoint.
The MIND trial found that evacuation of the hematoma using the Artemis neuro evacuation device had a high technical success rate with substantial hematoma reduction, and although there was early clinical improvement in disability scores compared with medical management alone, these were not sustained out to 6 months.
However, the study was stopped early, so was underpowered to show significant effects.
The MIND trial was presented on February 5 at the International Stroke Conference (ISC) 2025.
No Signal of Harm
It follows on from the recently reported ENRICH trial — the first positive trial of minimally invasive surgery in patients with ICH.
“Our results build on those from the ENRICH trial, showing some positive effects, with no signal of harm,” lead investigator David Fiorella, MD, Stony Brook University Hospital, Stony Brook, New York, told Medscape Medical News.
“We showed some early benefits with the minimally invasive surgical procedure. Consistent with the ENRICH trial, there appeared to be a greater effect in patients with lobar ICH vs those with deep ICH. These results are very encouraging for future studies of this technique,” he added.
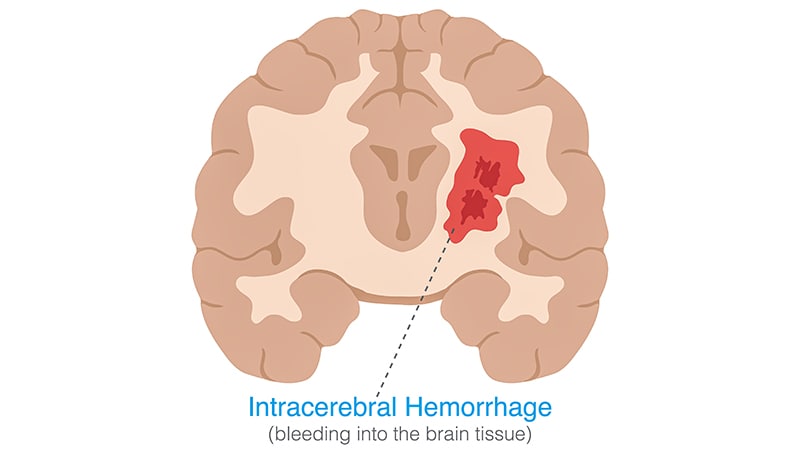
Fiorella explained that spontaneous ICH is a relatively common experience, with around 80,000 cases per year in the United States. Blood leakage from a ruptured cerebral blood vessel into the brain parenchyma causes brain injury, and these patients have a mortality rate of 30%-40%. There is a large unmet need in this field, and despite considerable health and economic burden, the majority of patients with ICH are left without any definitive treatment, he said.
In patients who have a large life-threatening bleed, open brain surgery can be undertaken to remove the hematoma to try and preserve survival, but trials of open surgery in more moderate spontaneous bleeds (STICH trials) have failed to show a benefit.
A novel strategy is now being investigated with the use of devices that allow a minimally invasive approach to surgery to drain the hematoma.
Minimally Invasive Approach
The ENRICH trial, which was published last year, was the first study to show a benefit with such an approach using a trans-sulcal technique that allows neurosurgeons to access the brain through natural folds in the cerebral cortex.
The MIND trial evaluated a different device for the minimally invasive surgical approach using the Artemis evacuation device employed via cranial access utilizing a 14-mm burr hole.
The MIND trial planned to include 500 patients with moderate to large volume supratentorial ICH (20-80 mL), presenting within 24 hours of symptom onset, who were randomized to the minimally invasive surgical procedure or best medical therapy alone within 72 hours of the bleed.
However, after the ENRICH trial reported benefits with a minimally invasive surgical technique in patients with lobar ICH, the clinical equipoise of MIND was in question, and enrollment of patients was stopped after 236 patients had been enrolled, leaving the trial underpowered.
Of these patients, 82 were allocated to the medical treatment arm and 154 to the minimally invasive surgery arm. The majority of patients (70%) presented with ICH in primarily deep locations and 30% had lobar bleeds.
Approximately, one third of patients had ICH with intraventricular involvement. The median time to the procedure was 27 hours from symptom onset.
Fiorella noted that the procedure showed excellent rates of hematoma evacuation of around 80% in both patents with deep and lobar ICH and was quick to perform with an average procedure time of 27 minutes (37 minutes for deep ICH and 25 minutes for lobar ICH). The rate of conversion to craniotomy was very low at 1.4%.
The primary endpoint was 180-day global disability assessed using the ordinal modified Rankin score. This showed no difference between the two groups with an odds ratio of 1.03.
However, the surgical group showed a more favorable clinical outcome at 30 days, and Fiorella said this early beneficial effect was consistent with the ENRICH trial.
Mortality rates at 30 days were much lower than expected in both arms — 9.8% with medical management vs 7.2% with minimally invasive surgery, a nonsignificant difference.
Benefit in Lobar ICH?
Fiorella noted that the medical treatment arm showed a mortality rate of around half of that reported in the literature for a similar patient population.
However, there was a numerical, but not significant, reduction in mortality with the surgical approach in patients with lobar ICH — 22.7% medical vs 8.3% minimally invasive surgery.
There was also a lower rate of serious adverse events at 180 days in the surgical group (68% medical vs 52% surgery), which was more marked in patients with lobar ICH.
In particular, Fiorella highlighted a lower incidence of edema in the minimally invasive surgery arm (2.6% vs 13.4% in the medical care alone arm), which suggested reduced secondary injury (without increased bleeding risk).
Fiorella pointed out that the MIND trial recruited mainly patents with deep ICH, but the minimally invasive surgical technique seems to work better in patents with lobar ICH.
He also suggested that better results may have been obtained if the procedure had been conducted earlier.
“The ENRCH and MIND trials together suggest that the minimal invasive surgery approach is more likely to be beneficial in lobar ICH patients,” he said.
Early Days
Commenting on the MIND trial for Medscape Medical News, Craig Anderson, MD, The George Institute for Global Health, Sydney, Australia, said it was unfortunate that the trial was stopped early.
“Because of the early termination, the study is very underpowered, so the results are just descriptive. There are some trends toward benefit, but nothing significant.”
Anderson noted that although the ENRICH trial showed “remarkably positive results,” this minimally invasive surgical approach has not become widely adopted yet.
“It can be challenging to incorporate new surgical techniques into routine practice. This is a complex intervention. Hospitals have to invest in the equipment, and surgeons have to train in the new procedure,” he added.
Fiorella responded that the minimally invasive surgical approach is a new technique, with data from ENRCH still being digested.
“This strategy is in the early stages of evolution. With more data from our study and future studies, we will get better at identifying the patients who will benefit from this approach, and I expect that practice will gradually change over time,” he said.
The MIND trial was sponsored by Penumbra, Inc., the manufacturer of the Artemis device. Fiorella reported receiving consulting fees from Medtronic, Stryker, Balt USA, Cerenovus, RAPID Medical, Q’apel, phenox, Mentice, and MicroVention and having shareholdings in Scientia, Arsenal, and Elixir.
[ad_2]
Source link : https://www.medscape.com/viewarticle/minimally-invasive-surgery-ich-more-encouraging-data-2025a10003jo?src=rss
Author :
Publish date : 2025-02-11 13:31:10
Copyright for syndicated content belongs to the linked Source.