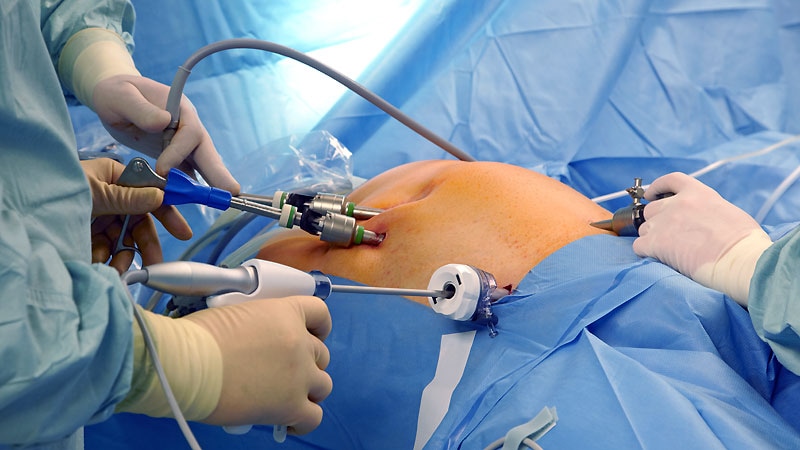
New data suggested that laparoscopic radical hysterectomy that uses modified tumor-free (MTF) techniques can improve outcomes for patients with early-stage cervical cancer.
An editorialist, however, urges caution in using these techniques for cervical cancer outside of a clinical trial setting.
Study authors, led by Yuan Li, MD, with the National Clinical Research Center for Obstetric & Gynecologic Diseases in Beijing, China, conducted a retrospective cohort study of 276 patients with early-stage cervical cancer who were treated at a single, high-volume center between January 2017 and January 2023.
The group included 151 patients who underwent laparoscopic radical hysterectomy that incorporated MTF techniques (MTF group) and 125 patients who underwent conventional laparoscopic radical hysterectomy with a uterine manipulator and unprotected intracorporeal colpotomy (non-MTF group). Findings were published in the February edition of Obstetrics & Gynecology.
The researchers concluded that the modified approach is feasible and leads to better outcomes than conventional laparoscopic radical hysterectomy. The MTF technique relies on suspension of the uterine fundus instead of using a manipulator and enclosed colpotomy with either sterile cable tie or cerclage suture. With the modified version, before colpotomy, surgeons used one of the two approaches to protectively close the upper vagina to isolate the cervical tumor.
The authors noted that two major concerns regarding the safety of minimally invasive surgery have been the use of uterine manipulators and unprotected colpotomy.
Li’s team found that after 24 months of follow-up, the cervical cancer recurrence rates was 0.7% in the MTF group and 8% in the non-MTF group. Their respective 2-year disease-free survival (DFS) rates were 99.3% and 91.9%.
“In the primary analysis limited to 2-year survival, the adjusted multivariate analysis showed that use of modified tumor-free techniques was an independent predictor of longer DFS (hazard ratio, 0.10; 95% CI, 0.01-0.77; P = .027). After inverse probability treatment weighting, patients in the MTF group had a more favorable DFS than those in the non-MTF group (log-rank P = .031),” the authors wrote.
Additionally, patients in the MTF group had a shorter length of hospital stay than those in the non-MTF group (6 days vs 7 days; P
Editorialist Urges Caution
In an accompanying editorial, Jason D. Wright, MD, with the Department of Obstetrics & Gynecology at Columbia University College of Physicians & Surgeons in New York City and editor in chief of Obstetrics & Gynecology, said that though the results by Li and colleagues are intriguing, caution should be exercised with the use of minimally invasive radical hysterectomy for cervical cancer.
He pointed out that the Laparoscopic Approach to Cervical Cancer trial, which called into question the safety and outcomes of minimally invasive laparoscopic hysterectomy for cervical cancer, “also called into question the ability of minimally invasive surgery to reduce the morbidity of radical hysterectomy, the impetus for development of the procedure in the first place.”
Wright pointed to limitations of the Li study, such as underlying selection bias, which the authors acknowledged, as patients with more favorable oncologic factors underwent MTF radical hysterectomy. The study also had a small sample size with limited follow-up, he noted, and procedures were performed by a small number of surgeons “at a very high-volume center.”
The authors also noted that there were significant differences in average age between the two groups (44.1 years [MTF group] vs 47.0 years [non-MTF group]; P = .013), number with stage II disease (3.3% vs 10.4%; P = .033), and lymph node metastasis (8.6% vs 20.0%; P = .011).
Wright added that discussions with patients are critical in weighing the risks for and benefits of the procedure. Future studies should incorporate patient-reported outcomes, he said.
“Although minimally invasive radical hysterectomy still may find a role in the treatment of cervical cancer,” he wrote, “the procedure serves as a reminder that innovation must be accompanied by evidence.”
The study was supported by the National Natural Science Foundation of China, CAMS Innovation Fund for Medical Sciences, and National High Level Hospital Clinical Research Funding. Authors reported no relevant financial relationships. Wright received research support from Merck and honoraria from UpToDate and the American College of Obstetricians and Gynecologists.
Marcia Frellick is an independent healthcare journalist based in Chicago.
Source link : https://www.medscape.com/viewarticle/can-modified-laparoscopic-radical-hysterectomy-improve-2025a10001nv?src=rss
Author :
Publish date : 2025-01-23 12:08:06
Copyright for syndicated content belongs to the linked Source.