Final survival results from the WSG ADAPT hormone receptor–positive (HR+)/human epidermal growth factor receptor 2–negative (HER2–) chemotherapy trial demonstrated that weekly nanoparticle albumin-bound (nab)-paclitaxel improved disease-free survival specifically in patients with HR+/HER2– early breast cancer who had low recurrence scores (RS) and did not respond to endocrine therapy.
“The ADAPT trial established that the combination of clinical risk, genomic risk, and endocrine response allows optimal patient selection for endocrine therapy or chemotherapy in HR+/HER2– early breast cancer,” said author Sherko Kuemmel, MD, during his presentation at the San Antonio Breast Cancer Symposium 2024. Kuemmel is Clinical Director and Chairman of the Interdisciplinary Breast Unit Clinics of Essen-Mitte, Germany.
The phase III trial, which enrolled 2233 patients, compared two dose-dense chemotherapy regimens: Weekly nab-paclitaxel (125 mg/m2 for eight cycles) vs biweekly solvent-based paclitaxel (175 mg/m2 for four cycles), both followed by epirubicin and cyclophosphamide every 2 weeks.
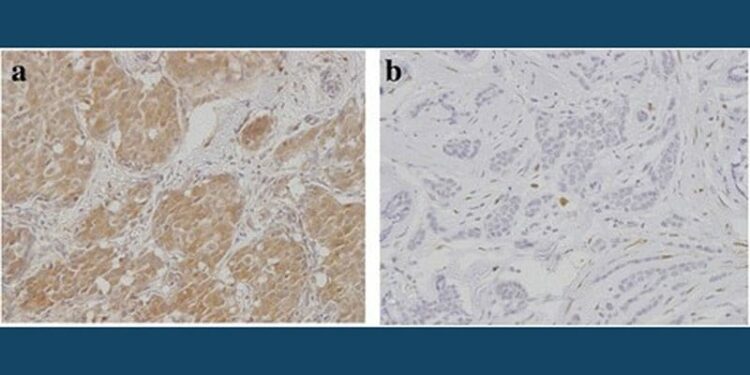
The trial enrolled patients with high-risk features, including those with 0-1 positive nodes and RS of 12-25 who showed poor response to endocrine therapy (posttreatment Ki67 > 10%), patients with RS > 25 regardless of endocrine response, and those with N2-3 disease or other high-risk features such as grade 3 disease or Ki67 > 40%.
“What we learned from the ADAPT data program is that patient selection using both recurrence score in combination with endocrine response to determine dynamic Ki67 expression is feasible in clinical practice,” Kuemmel noted.
Nab-paclitaxel Improves Invasive Disease-Free Survival but Not Overall Survival
The trial showed a trend toward improved 5-year invasive disease-free survival (iDFS) with nab-paclitaxel compared with solvent-based paclitaxel (85.7% vs 82.9%, P = .054). Disease-free survival (DFS) and relapse-free survival (RFS) showed significant advantages with nab-paclitaxel over solvent-based paclitaxel, with 5-year DFS rates of 84.9% vs 81.7% (P = .035) and 5-year RFS rates of 86.9% vs 84.0% (P = .041).
Subgroup analyses revealed that the benefit of nab-paclitaxel was primarily observed in patients with RS ≤ 25, particularly among endocrine therapy nonresponders (5-year iDFS: 89.5% vs 84.5%, P = .011). In contrast, no significant advantage was observed in patients with RS > 25 (5-year iDFS: 82.9% vs 82.7%).
However, improvement in disease-free survival did not translate to significant advantages in distant DFS (dDFS) or overall survival (OS). The 5-year dDFS rates were 87.1% vs 84.8% (P = .13), and the 5-year OS rates were 94.0% vs 92.9% (P = .387).
Nan Chen, MD, assistant professor at the University of Chicago, who was not involved in the study, offered a measured interpretation of the findings.
“This study evaluated two different schedules of taxanes and found that the weekly schedule of nab-paclitaxel may improve outcomes. This weekly schedule is standard for many providers and institutions, including myself,” she noted in an interview with Medscape Medical News.
Chen cautioned against changing how doctors treat patients with lower RS based on this study.
“We typically think of patients with RS
Regarding the practical implications of switching to weekly nab-paclitaxel, Chen pointed out potential challenges: “There is an increase in chair time and lab tests, among other things, which certainly have a financial cost. Furthermore, patients may experience more time and financial burden by having to come to the clinic twice as much.”
The safety profiles of nab-paclitaxel and solvent-based paclitaxel were generally manageable, with similar discontinuation rates due to adverse events in both arms (7.9% with paclitaxel vs 7.8% with nab-paclitaxel). More grade ≥ 3 events and hematologic toxicities were observed with nab-paclitaxel, although there was less neuropathy than with conventional paclitaxel.
Implications and Future Directions
Kuemmel emphasized that the ADAPT trial represents the largest prospective study comparing two taxane-based dose-dense regimens in patients selected by recurrence score and endocrine response, and that the findings add important nuance to ongoing discussions about optimizing chemotherapy regimens in HR+/HER2– early breast cancer.
During his presentation, Kuemmel noted that the fully recruited ADAPTcycle trial will investigate whether chemotherapy can be replaced by CDK4/6 inhibitor-based regimens in intermediate to high-risk HR+/HER2– early breast cancer, with the first results expected in 2027.
Although the final results from the ADAPT trial suggest potential advantages of weekly nab-paclitaxel, particularly in endocrine nonresponsive tumors with lower RS, Chen said that the lack of OS benefit and the increased burden of weekly administration require careful consideration in treatment decision-making.
Chen also emphasized the evolving landscape of the management of HR+/HER2– early breast cancer.
“We really need to better understand the ideal chemotherapy regimen for these patients, and it may be different depending on both clinical and genomic risk. CDK4/6 inhibitors in the adjuvant setting will likely change how we think about which patients may need chemotherapy, and certainly, novel drugs such as antibody-drug conjugates will also change our use of chemotherapy in this patient population,” she said.
The study was funded by Exact Sciences, AMGEN, BMS/Celgene, NanoString, Bayer, and AOK. Kuemmel reports receiving grant funding from Roche and Novartis; speaker’s bureau fees from Novartis; and honoraria or consultant fees from AstraZeneca, Celgene, Daiichi Sankyo, Genomic Health / Exact Sciences, Lilly, Novartis, Seagen, Pfizer, Roche, Hologic, Gilead, MSD Oncology, Sonoscape, Agendia, Pink, and Stemline. Chen reported receiving consultant fees from Guardant Health, Daiichi Sankyo, Stemline, Seagen, AstraZeneca, and Novartis.
Christos Evangelou, PhD, is a freelance medical writer and science communications consultant.
Source link : https://www.medscape.com/viewarticle/weekly-nab-paclitaxel-shows-modest-advantage-high-risk-hr-2024a1000ojm?src=rss
Author :
Publish date : 2024-12-19 08:56:13
Copyright for syndicated content belongs to the linked Source.