CHICAGO — Two early-phase clinical trials released data at the American Society of Clinical Oncology (ASCO) 2025 annual meeting that suggest their premise — an elranatamab-based triplet regimen and a new trispecific regimen — shows good potential in multiple myeloma (MM).
“It was interesting to see where these new lines of thought will take us in treating myeloma. Elranatamab is already approved in the third-line setting in the US, and using it in the frontline setting in MagnetisMM-6 shows promise,” said oral abstract session discussant Amrita Krishnan, MD, of the City of Hope Comprehensive Cancer Center in Duarte, California. “And the first-in-human data from JNJ-5322 shows the drug has incredible activity.”
“In both these trials, we need to see if their responses hold,” Krishnan added.
Early MagnetisMM-6 Readout
The key takeaway from MagnetisMM-6 Part 1, dose level G, is that initial data show that the triplet combination of elranatamab with daratumumab and lenalidomide is effective and manageable in patients with newly diagnosed MM who are not eligible for transplant. That’s according to study author Hang Quach, MD, of St Vincent’s Hospital Melbourne, University of Melbourne, in Melbourne, Australia.
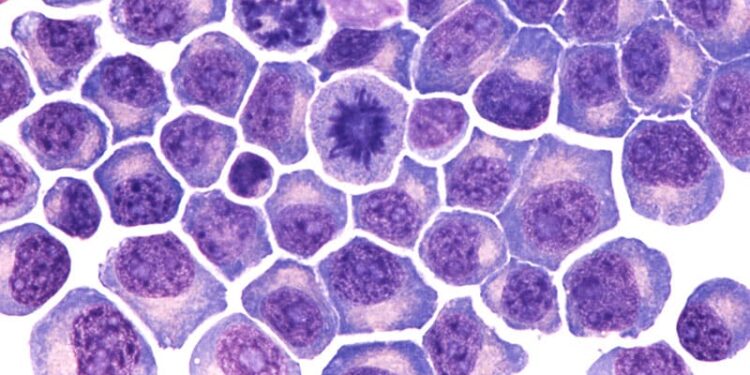
Elranatamab is a B-cell maturation antigen (BCMA)-CD3 bispecific antibody approved as a late-line monotherapy in relapsed or refractory multiple myeloma. Quach and co-authors hypothesized that adding daratumumab and lenalidomide may enhance immune cell-mediated myeloma cell death.
MagnetisMM-6 enrolled 37 patients with transplant-ineligible newly diagnosed MM. Of these, 34 received the triplet regimen. At data cutoff, the median follow-up was 7.9 months, and 32 patients were still on treatment. “The combination showed early and promising efficacy, and we expect responses to deepen with longer follow-up,” Quach said.
Quach reported that the safety profile was predictable and consistent with the components’ known toxicities. Treatment-related adverse events were seen in more than 50% of patients. The most common were hematologic AEs, infections, and cytokine release syndrome (CRS). All CRS events were grade 2 or less, and one grade 2 immune effector cell-associated neurotoxicity syndrome event occurred.
The phase 3 MagnetisMM-6 Part 2 trial, which will open soon, will evaluate the same elranatamab triplet combination against daratumumab plus lenalidomide plus dexamethasone in transplant-ineligible and transplant-deferred patients with newly diagnosed MM. The study design is patient-centric regarding dosing frequency and de-escalation, Quach said: “There will be a response-adapted scheduling modification upon achievement of complete response after 12 months at least.”
JNJ-5322: First-in-Human Trial
The first-in-human trial of JNJ-5322, a BCMA- and GPRC5D-targeted T-cell redirecting trispecific antibody, enrolled 147 patients. “We treated these patients with different doses and at different dosing schedules and defined the recommended phase 2 dose (RP2D) as 100 mg administered every 4 weeks subcutaneously with only one step-up dose,” said Niels W.C.J. van de Donk, MD, PhD, of Amsterdam University Medical Center, Vrije Universiteit Amsterdam, Amsterdam, the Netherlands. “At the RP2D, we see a manageable safety profile with improved or similar GPRC5D-related adverse events.”
As expected, infections were common. The grade 3 or 4 infection rate was 28.6% with prophylactic infection management.
GPRC5D-related oral side effects were also observed in the study. Taste-related changes were observed in 60% of patients, while other non-taste-related oral AEs were less frequent and included dry mouth, dysphagia, stomatitis, and decreased appetite. “The frequency and severity of these oral adverse events is lower than what is typically seen,” van de Donk said. “And this milder oral treatment emergent AE profile is also reflected in that only 6% of the patients had a transient weight loss of grade 1 or grade 2.”
Among patients naive to BCMA- and GPRC5D-targeted therapies and treated at the RP2D, the investigators observed a 100% response rate, a complete response (CR) rate of 70%, and at least a very good partial response in 96%. “And this deep response translates into a promising progression-free survival of 95% at 1 year,” van de Donk said. “Overall, JNJ-5532 demonstrated a manageable safety profile and an overall response rate comparable to CAR [chimeric antigen receptor] T with convenient off-the-shelf every 4 weeks dosing with one step-up dose to facilitate outpatient dosing.”
Following this presentation, Krishnan sat down with Medscape Medical News. The following interview has been edited for clarity.
What is the premise of the MagnetisMM-6 trial?
The rationale for using elranatamab in the upfront, newly diagnosed setting is that, in a newly diagnosed myeloma, you probably have healthier T cells than a patient with heavily pretreated disease. The hope is that this drug may work even better in this setting.
What stood out to you about MagnetisMM-6’s trial design?
Participants had a median age of 75 years, which is old for a trial, and 24% of them were frail, which is also quite notable. Patients had a very deep response, which is encouraging in this newly diagnosed setting. The approved dose of elranatamab is weekly, but the investigators gave it only once every 4 weeks, which may be in part why they had a much more favorable safety profile in terms of risk for infection.
What will you be watching for from MagnetisMM-6?
The data looked promising, but the follow-up is very short. On this trial it’s about 7.9 months, so we really need to see if the responses hold and how deep the responses are.
What is the premise of the JNJ-5532 trial?
The drug targets both GPRC5D and BCMA, with the idea being that, if you hit both targets at once, maybe your response rates are higher than hitting just one target, and that appears to be the case. The reported response rates of 100% are certainly dramatic, but the follow-up right now is very short.
What stood out to you about JNJ-5532?
With most of the bispecifics, the response rates are about 60%-70%. Now we’re looking at a response rate that’s close to CAR T-cell therapy for the first time, and it’s frankly incredible. But the attractive thing with CAR T has always been “one and done” vs staying on treatment for a fixed duration or even indefinitely. If you’re still having to give patients a drug for, say, 5 years, that’s probably not as attractive.
Is JNJ-5532 likely to be better tolerated than CAR T?
We haven’t seen any neurologic toxicity yet, so that’s encouraging. And the logistics, of course, are much easier. With JNJ-5532, you get one step-up dose, and it can be given outpatient. So, the comparison with CAR T is not just about side effects: The whole burden of care is very different, and the ability to get it in the community versus entirely inpatient is another big issue in terms of access.
MagnetisMM-6 was funded by Pfizer. Quach disclosed relationships with Antengene (Inst), Amgen, Bristol Myers Squibb/Celgene, Celgene, GlaxoSmithKline (Inst), Janssen-Cilag, Karyopharm Therapeutics (Inst), Pfizer, roche, and Sanofi (Inst).
JNJ-5532 was funded by Johnson & Johnson. van de Donk reported ties with Adaptive Biotechnologies (Inst), Amgen (Inst), Bayer (Inst), Bristol Myers Squibb Foundation (Inst), Celgene (Inst), Cellectis (Inst), Janssen (Inst), Merck (Inst), Novartis (Inst), Roche (Inst), Servier (Inst), and Takeda (Inst).
Darcy Lewis (https://www.darcylewis.com/) writes about clinical medicine from Chicago.
Source link : https://www.medscape.com/viewarticle/q-new-myeloma-bispecific-rivals-car-t-early-data-2025a1000g9r?src=rss
Author :
Publish date : 2025-06-18 13:10:00
Copyright for syndicated content belongs to the linked Source.