[ad_1]
The results of the global phase 3 LAPIS trial suggest that the addition of pamrevlumab to standard chemotherapy fails to improve survival outcomes in patients with locally advanced pancreatic cancer (LAPC) despite promising early-phase results.
The findings highlight the ongoing challenges in developing effective treatments for this aggressive disease, according to lead investigator Vincent J. Picozzi, MD, of Virginia Mason Hospital and Medical Center in Seattle.
“LAPIS is an important study for the future of locally advanced pancreatic cancer despite not meeting its primary endpoint,” said Picozzi during his presentation of the results at the Gastrointestinal Cancers Symposium (GICS) 2025.
He added that the trial’s novel methodology and comprehensive approach to assessment may help inform the design of future studies in LAPC.
“A deeper dive into the data, I believe, will provide significant insights into the challenges in treating LAPC and opportunities for future studies,” he explained.
Study Rationale and Design
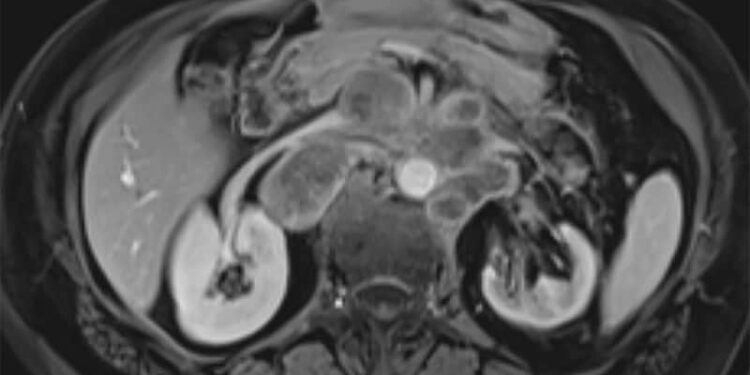
Pamrevlumab, a fully humanized monoclonal antibody targeting connective tissue growth factor, had shown encouraging results in phase 1 and 2 trials. In his presentation, Picozzi explained that the LAPIS trial (NCT03941093) was designed to definitively evaluate the efficacy of pamrevlumab when combined with standard chemotherapy in treatment-naive patients with unresectable LAPC.
“This was a large global trial with key trial innovations, including objective criteria for surgical decision-making, CA19-9 monitoring, FDG [fluorodeoxyglucose]-PET imaging, radiographic review, and expert surgical panel review,” Picozzi said.
The innovative design elements of the LAPIS trial, including pre- and post-chemotherapy FDG-PET imaging and objective criteria for surgical intervention, may serve as a template for future studies, said Flavio G. Rocha, MD, professor and division head of Surgical Oncology at Oregon Health and Science University, Portland, Oregon, who was not involved in the trial.
“I think these are important innovations that should be incorporated into future trials,” Rocha said. “To those, I would add staging laparoscopy, which was suggested but not mandated in this study, to rule out micrometastatic disease and better biomarkers to determine response during neoadjuvant therapy.”
The double-blind, placebo-controlled trial randomized 284 patients (143 pamrevlumab, 141 placebo) to receive either pamrevlumab (35 mg/kg Q2W) or placebo plus investigator’s choice of chemotherapy — either gemcitabine plus nab-paclitaxel (approximately 80% of patients) or FOLFIRINOX (approximately 20%) — for up to six 28-day cycles.
Similar Survival Outcomes in Both Groups
Overall survival, the primary endpoint of the study, showed no significant difference between the two groups, with a median overall survival of 17.25 months (95% CI, 15.47-18.89) in the pamrevlumab group vs 17.94 months (95% CI, 14.59-20.34) in the placebo group (hazard ratio, 1.08; 95% CI, 0.83-1.41; P = .55). Secondary endpoints, including event-free survival and progression-free survival, also showed no significant differences between the groups.
Notably, the objective response rate was lower in the pamrevlumab group (30.1%) than in the placebo group (45.4%). All responders in both groups showed partial response.
Rocha offered several potential explanations for this finding: “The lower objective response rate in the experimental arm is puzzling but may be related to a few factors. The LAPIS trial allowed for gemcitabine/nab-paclitaxel and FOLFIRINOX, while the previous trial was only with gemcitabine/nab-paclitaxel. The evaluation was also done centrally, as opposed to locally.”
Rocha also provided insights into the disconnect between early- and late-phase trial findings.
“The initial trial was focused on a single institution with a limited number of patients, and the primary endpoint was eligibility for resection, whereas this confirmatory study had more robust objective criteria for surgical intervention and included surgeons worldwide.”
Surgical Outcomes and Safety
Approximately two thirds of the patients completed all six treatment cycles. Among the 69 patients deemed potentially reconstructable at treatment outset, surgical outcomes were similar between groups, with 15%-20% meeting objective criteria for surgery and approximately 9% achieving successful R0 or R1 resection.
The safety profile was generally comparable between the groups for patients receiving gemcitabine/nab-paclitaxel. However, in the FOLFIRINOX cohort, respiratory, thoracic, and mediastinal disorders (39.3% vs 27.6%) and skin and subcutaneous tissue disorders (53.6% vs 37.9%) occurred more frequently with pamrevlumab. One treatment-related death was reported in the pamrevlumab group.
Study Limitations and Future Directions
During his presentation, Picozzi acknowledged several important limitations of the study, including that it was conducted internationally with variations in how patients were managed, particularly with respect to supportive care.
“The inclusion of patients with nonreconstructable disease, which was about 70% of the total patient population, may have limited the potential for curative resection survival,” he said.
Picozzi added that the trial having been conducted during the COVID-19 pandemic may have influenced survival outcomes.
Despite the negative results, “the median overall survival of 17-18 months observed in both arms seems relatively good for LAPC,” Rocha said.
“The ability to perform aggressive resections in this population after a period of response and stability on induction therapy probably has extended the survival the most in this population. When I started my training, LAPC was always thought to be unresectable, and today, we are always trying to find ways to get these patients to surgery,” he said in an interview.
Regarding future therapeutic directions, Rocha expressed cautious optimism.
“Newer agents that are able to convert unresectable to potentially resectable disease followed by preventing recurrence postoperatively will yield the most promising results. I’m hopeful that some of the newer KRAS inhibitors and others that target inherent pancreatic cancer biology may fulfill this role, but they do need to be studied in the localized setting,” he said.
This study was independently supported. Picozzi reported receiving consulting or advisory fees from TriSalus Life Sciences; stock and other ownership interests from Amgen, Cigna, Iovance Biotherapeutics, Johnson & Johnson, McKesson, and Thermo Fisher Scientific; and research funding from Abbvie, Amal Therapeutics, Astellas Pharma, FibroGen, Ipsen, NGM Biopharmaceuticals, and Novocure. Rocha reported receiving consulting or advisory fees from AstraZeneca, Medtronic, Histosonics, and Oncosil; and payments related to travel, accommodation, or expenses from Lynx Group.
Christos Evangelou, PhD, is a freelance medical writer and science communications consultant.
[ad_2]
Source link : https://www.medscape.com/viewarticle/novel-anti-ctgf-antibody-plus-chemotherapy-shows-no-survival-2025a100027u?src=rss
Author :
Publish date : 2025-01-29 11:30:33
Copyright for syndicated content belongs to the linked Source.