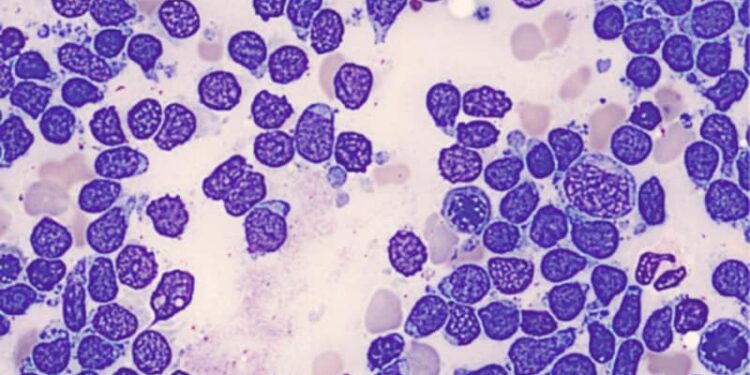
In the treatment of newly diagnosed Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ ALL), patients who fail to achieve initial molecular response with the third-generation tyrosine kinase inhibitor (TKI) ponatinib following induction can nevertheless go on to achieve minimal residual disease (MRD) negativity — and at higher rates than the earlier generation TKI imatinib.
“These results support the clinical benefit and tolerability of continuing ponatinib beyond cycle 3 in patients with newly diagnosed, Ph-positive ALL who do not achieve MRD-negativity by the end of induction,” first author Ibrahim Aldoss, MD, of City of Hope hospital in Duarte, California, told Medscape Medical News.
The study was presented this week at the 2025 American Society of Clinical Oncology (ASCO) Annual Meeting.
Ph+ ALL, the most common subtype of adult ALL and once associated with a particularly poor prognosis, has seen significantly improved outcomes with TKIs in combination with chemotherapy or steroids. However, even with the third generation of TKIs representing the standard of care, relapses can occur due to variant-acquired resistance, particularly T315I.
Ponatinib was designed to address that challenge, effectively inhibiting BCR-ABL1 with or without any single-mutation variants, including T315I.
The previous global, phase 3, open-label PhALLCON trial represented the first head-to-head comparison of ponatinib (30 mg/day) with the first-generation imatinib (600 mg/day), along with reduced-intensity chemotherapy followed by monotherapy of either drug until disease progression or unacceptable toxicity.
The trial met its primary endpoint of no sign of molecular disease (MRD-negative complete response), which correlates with long-term outcomes, by the end of cycle 3 of induction, with ponatinib showing a significantly higher rate vs imatinib (34.4% vs 16.7%; P = .002), and comparable safety outcomes.
Current Post-Hoc Analysis
To investigate the key question of the effects of further treatment among the majority of patients who did not achieve MRD negativity by the end of induction, or 3 cycles of low-density chemotherapy, Aldoss and colleagues conducted the current post-hoc analysis of 113 patients (73 receiving ponatinib, 40 imatinib) who continued treatment following the end of induction,
Of those patients, 48% in the ponatinib group (n = 35) and 33% with imatinib (n = 13) did achieve MRD negativity after induction cycle 4, day 1.
The median duration of MRD negativity was not reached with ponatinib compared with 3.8 months with imatinib treatment.
Overall, 16 patients (10 receiving ponatinib, 6 imatinib) went on to have a hematopoietic stem cell transplant (HSCT).
Among 140 patients who did not achieve MRD negativity by the end of induction, the median event-free survival was not reached with ponatinib therapy compared with 24.8 months with imatinib. The 2-year rates of event-free survival in the two groups were 82% and 62%, respectively.
The rates of treatment-emergent adverse events (TEAEs) were similar in the patients who had not achieved MRD negativity by the end of induction, at 100% with ponatinib and 98% imatinib.
In addition, 71% and 54% of patients, respectively, had a dose modification (discontinuation, reduction, or interruption) due to TEAEs.
Of the 48 patients with MRD negativity after cycle 4, day 1, 100% of patients in each treatment group had TEAEs, and 69% and 62% had dose modification due to TEAEs.
Vascular Toxicities Avoided With Lower Dose
While ponatinib has previously been associated with increased vascular toxicity and arterial occlusive events, particularly among patients receiving higher doses for longer periods, those events were rare in the current study and not significantly different between the two arms, Aldoss said.
He added that the improvement is likely the result of a lowering of the initial dose in the PhALLCON study to 30 mg/day compared with the prior use of 45 mg/day — and a further reduction to 15 mg/day after induction likely helped reduce those effects.
“We feel that using a more optimized, safer lower dose was actually the reason why we’re seeing comparable safety and lower arterial occlusive events in this study,” Aldoss said.
The benefits were observed across the evaluated subgroups, including patients older than age 60 years, which is important due to previous research showing some increased risk with ponatinib among older adults.
Benefits Extend to Older Patients
With more stringent criteria in the trial excluding patients with significant cardiovascular disease, Aldoss noted that, “if anything, the benefit was actually more prominent in patients older than 60.”
He therefore recommended consideration of that criteria in making patient selection.
Importantly, in the PhALLCON trial, the proportion of patients in the ponatinib arm who went on to receive HSCT was lower compared with imatinib, which could notably benefit older patients who may not respond as well to such treatment.
“The potency of ponatinib in combination with low-dose chemotherapy or no chemotherapy may render HSCT unnecessary for older or frail patients who achieve a 3-month MRD-negative complete remission,” the authors conclude in the study.
While the survival estimation can otherwise require long follow-up analysis, MRD negativity is increasingly seen as an important surrogate measure of long-term survival.
In one recent meta-analysis, MRD negativity at the end of induction had a significantly greater prognostic value in terms of event-free survival and long-term survival in patients with PH-positive ALL.
The current findings suggest such benefits may be achieved even when there is a delay in MRD negativity status after induction, Aldoss noted.
“This analysis supports [the conclusion] that a clinical benefit in event-free survival is observed, even if you don’t achieve the MRD negativity at the end of induction,” he said.
Following the publication of the PhALLCON trial, the US Food and Drug Administration granted ponatinib accelerated approval for the indication of Ph-positive ALL in March 2024.
In an accompanying editorial, Jacqueline S. Garcia, MD, of the Department of Medical Oncology, Dana-Farber Cancer Institute, Boston, Massachusetts, and colleagues speculated about the role of ponatinib in the context of other promising options.
“It is unclear whether PhALLCON’s ponatinib regimen will be preferred against second-generation tyrosine kinase inhibitors, especially regimens that incorporate blinatumomab or allosteric BCR-ABL1 inhibitors,” they write.
Importantly, with long-term data showing durable hematologic and molecular responses with combined dasatinib and blinatumomab, thereby offering a chemotherapy-free and toxicity-sparing induction and consolidation regimen, for instance, the option of ponatinib and reduced-intensity chemotherapy “may not be the optimal first choice for all Ph+ ALL patients,” they say.
A notable limitation of the study was that MRD was not assessed with next-generation sequencing (NGS), Pamela Sung, MD, PhD, an assistant professor in the Departments of Medicine and Pharmacology & Therapeutics, Roswell Park Comprehensive Cancer Center, Buffalo, New York, who co-moderated the ASCO session, told Medscape Medical News.
“NGS is more sensitive and specific than BCR-ABL1 PCR for B-ALL MRD detection,” she said. “It is increasingly being recognized that multi-lineage or ‘CML-like’ ALL exists, where patients are MRD-positive by BCR-ABL PCR but negative by NGS.”
Such patients have a similar relapse rate to those who are MRD-negative by both measures, but it is not known how many patients experience such discordance, Sung noted.
The findings are nevertheless important, not so much in showing the rate of MRD at a certain point in time, but the potential trajectory in MRD over the course of treatment, Sung noted.
“Typically, we would continue the current therapy regimen so long as the MRD is continuing to decrease,” she explained. “However, if unable to clear at the end of 1 to 2 cycles of consolidation, we would recommend allogeneic transplant if eligible.
“These new data support this strategy, using a high potency TKI with few deaths and relapses in the ponatinib arm (10%) for this subset of patients that were MRD-positive at the end of induction.
“Nearly half of patients converted to MRD-negative by the end of treatment with ponatinib, many of whom were negative at [a deeper molecular response] of MR4.5.”
The study was sponsored by Takeda Development Center Americas, Inc.
Aldoss disclosed relationships with AbbVie, Agios, Amgen, Jazz Pharmaceuticals, Kite Pharma, Syndax, Takeda, Pfizer, and Macrogenics. Sung reported no relevant financial relationships.
Source link : https://www.medscape.com/viewarticle/ph-all-post-induction-ponatinib-yields-molecular-response-2025a1000eqk?src=rss
Author :
Publish date : 2025-05-31 19:39:00
Copyright for syndicated content belongs to the linked Source.