TOPLINE:
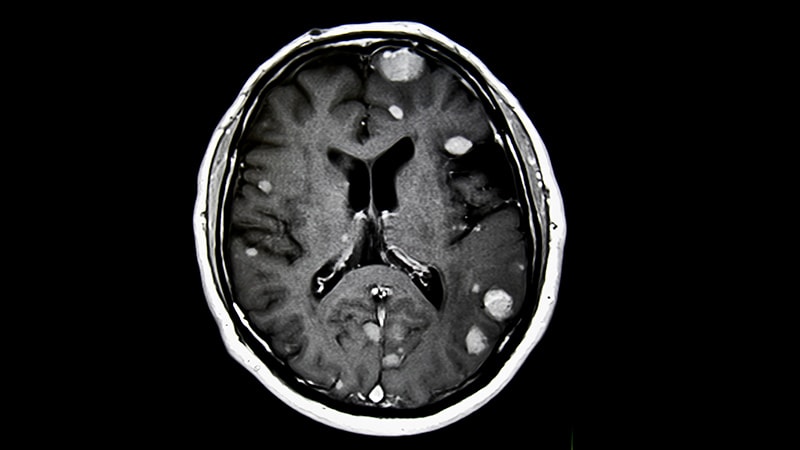
Patients undergoing stereotactic radiosurgery before resection of brain metastases demonstrated low rates of local recurrence, radionecrosis, and nodular leptomeningeal disease at 12 and 24 months, a new analysis found.
METHODOLOGY:
- For patients undergoing resection for brain metastases, postoperative stereotactic radiosurgery improves local control. However, radiosurgery after surgery comes with disadvantages, such as increased rates of leptomeningeal disease and radionecrosis. Providing radiation before surgery could help overcome these issues.
- The current analysis included 179 patients (with a total of 189 brain metastases) who underwent planned neoadjuvant stereotactic radiosurgery for brain metastases followed by resection. Patients were from nine institutions across five countries (Australia, Switzerland, South Korea, Canada, and the United States).
- Overall, 53% of brain metastases (100 of 189) underwent single-fraction neoadjuvant stereotactic radiosurgery, with a median dose of 18 Gy, and the remaining 47% underwent multi-fraction treatment. The most common dose for these patients was 24 Gy in three fractions (55%) or 27 Gy in three fractions (25%). The primary malignancies included non–small cell lung carcinoma (44%) and melanoma (17%).
- The primary endpoint was a composite of local recurrence, any grade radionecrosis, and nodular leptomeningeal disease. Distant brain failure and overall survival were also assessed. The median follow-up was 28.4 months.
TAKEAWAY:
- The 12-month incidence for the composite endpoint of local recurrence, any grade radionecrosis, and nodular leptomeningeal disease was 8.0% and the 24-month incidence was 12.3%. Distant brain failure was reported in 29.1% (39 of 134) patients at a median of 6.5 months. The 12-month overall survival rate was 66.3% and the 24-month overall survival rate was 48.2%.
- Local recurrence occurred in 12 metastases (6.3%) at a median of 7.3 months. The 12-month incidence was 4.6% and the 24-month incidence was 6.6%.
- Any grade radionecrosis occurred in 5.3% of brain metastases, at a median of 10.8 months. The 12-month incidence was 3.6% and the 24-month incidence was 4.4%. Five patients (2.6%) developed symptomatic radionecrosis at a median of 10.4 months, with a 12-month incidence of 1.8%.
- Leptomeningeal disease occurred in 17 patients (9.5%) at a median of 7.2 months. The 12-month incidence of leptomeningeal disease was 7.2% and the 24-month incidence was 11.0%.
IN PRACTICE:
This large international analysis provides further support to neoadjuvant stereotactic radiosurgery to treat brain metastases, with the study reporting low rates of local recurrence, leptomeningeal disease, and radionecrosis, the authors said.
SOURCE:
This study, led by Cristian Udovicich, of the Peter MacCallum Cancer Centre, Melbourne, Australia, was published online in Radiotherapy and Oncology.
LIMITATIONS:
A significant limitation was the absence of central review for imaging endpoints. The multi-institutional nature of the study led to variations in patient selection criteria and treatment protocols, including differences in dose fractionation, planning target volume margin, and timing of surgery. Additionally, there might have been incomplete reporting of non-radionecrosis toxicities.
DISCLOSURES:
No funding information was provided for the study. The authors declared that they had no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Source link : https://www.medscape.com/viewarticle/preoperative-radiosurgery-brain-metastases-shows-promise-2025a1000069?src=rss
Author :
Publish date : 2025-01-06 08:05:20
Copyright for syndicated content belongs to the linked Source.