[ad_1]
Chimeric antigen receptor (CAR) T-cell therapy has shown efficacy in blood cancers — with six CAR T-cell products now approved by the US Food and Drug Administration (FDA) to treat six hematologic malignancies.
For solid tumors, however, the efficacy of CAR T-cell treatments has been limited and progress “more incremental,” Christian Hinrichs, MD, with Rutgers Cancer Institute in New Brunswick, New Jersey, told Medscape Medical News. Currently, there are no CAR T-cell therapies approved in the United States to treat solid tumors.
Why have CAR T-cell therapies been less effective against solid tumors?
Perhaps the biggest hurdle is the ability to identify and selectively target specific molecular structures in cancer cells without causing severe toxicity by injuring healthy cells, Hinrichs and coauthors wrote in a recent JAMA review.
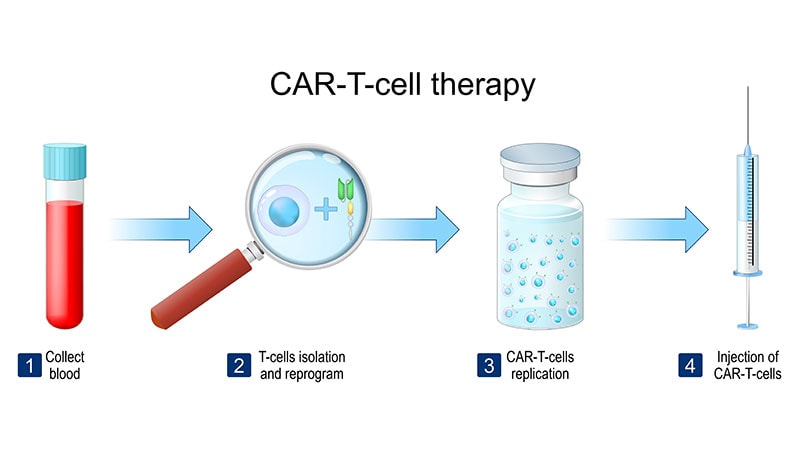
CAR T-cells are made up of “T cells genetically engineered to express a synthetic receptor that recognizes a tumor cell-surface protein,” Hinrichs and colleagues explained. But identifying cell surface antigens that are exclusive to solid tumor cells has been a challenge, which means CAR T-cell therapies end up affecting both tumor and healthy tissues.
“This makes it difficult to target and kill all the tumor cells without causing severe toxicity from injury to healthy cells,” Hinrichs explained.
Other common obstacles include challenges penetrating the dense extracellular matrix of solid tumors and the need to overcome inhibitory cells and molecules in the tumor microenvironment.
Despite the challenges and slow progress, some “promising results” have begun to emerge in the solid tumor, CAR T-cell space, Hinrichs said.
A recent phase 1-2 study, for instance, found that 63% (17 of 27) of pediatric patients with heavily pretreated neuroblastoma achieved an overall response with an investigational CAR T-cell therapy, GD2-CART01.
In a recent phase 1 trial, 38 of 98 patients with gastrointestinal cancers (39%) achieved partial or complete responses after receiving an investigational CAR T-cell treatment directed at Claudin18.2. However, the responses were short overall and could have been related to
the chemotherapy given before the CAR T-cell infusion.
Another phase 1 trial found that a GPC3-targeted CAR T-cell therapy led to an objective response rate in half (12 of 24) of heavily treated patients with advanced hepatocellular carcinoma, with a disease control rate of almost 91%.
Outside of CAR-T cell therapies, other cell-based treatments have shown promise against solid tumors, including two T-cell therapies recently approved by the FDA.
Last February, the FDA approved the tumor-infiltrating lymphocyte (TIL) therapy lifileucel (Amtagvi) for advanced melanoma. In August, the agency approved the T-cell receptor (TCR) therapy afamitresgene autoleucel for advanced synovial sarcoma.
“Response rates for these cellular therapies are in the 30% range, but already there is clear data that there’s durability for some patients, which is very exciting because previously treated patients really have very few treatment options,” Jennifer Brudno, MD, with the National Cancer Institute and co-author of the JAMA review, said in a journal podcast.
Several cell-based agents are in early trials to treat a range of solid tumors.
Hinrichs and colleagues previously reported findings from a phase 2 clinical trial of TIL therapy for human papillomavirus (HPV)–associated cancers including cervical, oropharyngeal, and anal cancers. Responses occurred in 5 of 18 patients with cervical cancer and 2 of 11 patients with noncervical cancers. “Two of the patients with cervical cancer had complete responses that are ongoing years after a single infusion of cells,” Hinrichs told Medscape Medical News.
Hinrichs was also involved in a phase 1 trial of gene-engineered TCR T-cells targeting HPV E7 for HPV-associated cancers reported tumor responses in 6 of 12 patients, including 4 of 8 with tumors refractory to checkpoint blockade immunotherapy. A phase 2 trial is now open at Rutgers Cancer Institute, as is an early trial testing a new TCR T-cell therapy targeting Kita-Kyushu Lung Cancer Antigen-1 to treat metastatic gastric, lung, breast, and cervical cancers.
Despite the encouraging findings, for CAR T-cell and other cell-based therapies to be successful against solid tumors, “we need to develop more treatments directed against antigens that are expressed by most or all the cells in a tumor but not by critical healthy tissues,” Hinrichs said.
“It may also be important to increase the potency of therapeutic cells and develop more sophisticated methods of antigen targeting that can better distinguish between tumors and healthy tissues,” he noted.
Brudno reported being an unpaid scientific advisory board member for and receiving travel expenses from Kyverna Therapeutics Inc. Hinrichs reported receiving personal fees from Neogene Therapeutics, Capstan Therapeutics, GlaxoSmithKline, Vir Biotechnology, and PACT Pharma, equity from Scarlet TCR (company officer), and sponsored research agreements from T-Cure Biosciences and Neogene Therapeutics outside the submitted work. He also holds several patents related to cellular therapies.
[ad_2]
Source link : https://www.medscape.com/viewarticle/promise-car-t-cell-therapies-solid-tumors-2025a10003by?src=rss
Author :
Publish date : 2025-02-10 11:59:02
Copyright for syndicated content belongs to the linked Source.