WASHINGTON, DC — A woman in her late 80s with mild dementia was recently referred to Vishal A. Patel, MD, director of cutaneous oncology at the George Washington (GW) Cancer Center, director of dermatologic surgery at the GW University School of Medicine and Health Sciences, and associate professor of dermatology and medicine/oncology at GW, Washington, DC, for discussion of Mohs surgery presented with a mixed basal cell carcinoma (BCC) — a superficial and nodular type — on the tip of her nose. She had a Mohs Appropriate Use Criteria (AUC) score of 8.

However, as Patel, the patient, and her daughter decided, Mohs wasn’t the best option, he recalled at the ElderDerm 2025 conference on dermatology in the older patient population. “A lot of us in the surgical world would say that’s a treatable, clearable, curable BCC [with Mohs surgery]. We can do it…very well. The question is, “should we do it,” Patel said.
“The Appropriate Use Criteria tell us whether a tumor is appropriate for Mohs, not whether it requires Mohs. You need to determine, with your patient, what is the best option,” he added.
Such cases are common in the growing population of older adults, where the incidence of nonmelanoma skin cancer is high and factors such as life expectancy, health status, and concern about the risk for additional morbidity should rightly — and more often — come into play, said Patel of GW, which hosted the meeting.
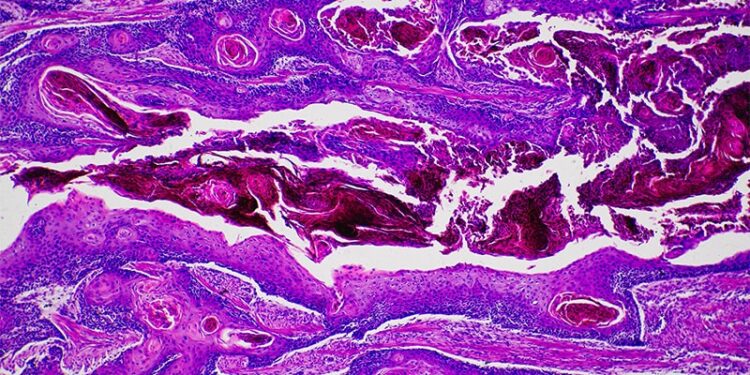
The high survival rates of BCC (5- and 10-year disease-specific survival rates above 99%) and cutaneous squamous cell carcinoma (SCC; 1-, 2-, 3-, 5-, and 10-year disease-specific survival rates of 99.6%, 97.9%, 95.3%, 93.6%, and 93.6%, respectively) should be part of the conversation, Patel said. Survival rates, he added, should be viewed “through the patient’s comorbidity lens.”
BCC “is a chronic disease and can be managed as such,” he said, “and even squamous cell carcinoma has survival rates above 90-plus percent and even higher when looking at early stages.” For melanoma, he added, the 5- and 10-year survival rates of stage 1A and stage 1B disease are also above 90% (99% and 98% in stage 1A disease and 97% and 94% in stage 1B disease).
Comprehensive risk assessment is key to informing the optimal therapy decision for patients with limited life expectancy, where the morbidity and mortality risk associated with skin cancer are unlikely to affect the patient, Patel said.
Underutilized in the older population is the option of shave removal for low-risk SCCs and BCC, as stipulated in the National Comprehensive Cancer Network (NCCN) guidelines, he said. Alternatively, he noted, “disc shave or scoop excision at the time of the initial biopsy may be an even more effective way” to manage low-risk disease in older adults, effectively clearing the lesion and avoiding potential follow-up.
For Patel’s patient, topical imiquimod was deemed to be the preferred treatment for the 1-cm tip-of-nose lesion. The patient and her daughter were concerned about the potential for a complicated reconstruction after Mohs surgery and “wanted the least invasive option possible,” said Patel.
They wanted to reserve the option of surgery if the nonsurgical option was not effective, he said, and given her age and comorbidities, “they were content with the potential risk of an inferior clearance or cure rate that would come with that.”
The patient lives in an assisted living facility, has no family history of melanoma or keratinocyte carcinomas, and has Fitzpatrick type II skin with a history of blistering sunburns as a child, he noted.
Supporting Data and the Patient’s Response to Imiquimod
Supporting that decision-making process was a randomized controlled trial published in 2017 comparing surgery with imiquimod 5% cream for nodular and superficial BCC, showing that imiquimod was inferior to surgery but still provided sustained benefit, Patel said.
The 5-year success rates (absence of recurrence) in that trial were 82.5% compared with 97.7% for surgery (relative risk of imiquimod success, 0.84; 95% CI, 0.77-0.91; P < .001) — rates that were comparable to previously reported 3-year success rates of 83.6% and 98.4% for imiquimod and surgery, respectively. Most recurrences occurred within the first year.
The “caveat,” Patel said, was that the trial looked only at low-risk locations such as the cheek and the trunk, and not the tip of the nose. Patients with superficial BCC received 6 weeks of imiquimod cream once daily, and those with nodular BCC received 12 weeks. Use of this therapy “requires clear explanation to the patient and an understanding of the off-label and not-fully-evaluated potential application,” Patel said in an interview after the meeting.
After 6 weeks of treatment, the patient had notable crusting of the nasal tip with surrounding erythema. At 12 weeks, the tip of her nose was “smooth with no obvious residual carcinoma notable,” Patal said at the meeting. “She tolerated the treatment well and had a great response.”
There have been suggestions made among some Mohs surgeons that the Mohs surgery AUC for primary superficial BCCs should be reevaluated, Patel said, referring to a Viewpoint piece published in JAMA Dermatology in July 2018 that pointed out that they are indolent, penetrate minimally, and are often multifocal, making them amenable to nonsurgical treatments. The lower-risk nodular BCC subtype is also worthy of AUC reevaluation, he said.
Decision-Making About a Second Lesion: Melanoma In Situ (MIS)
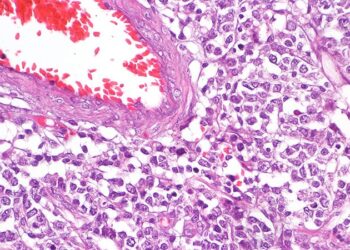
During the follow-up period, the patient’s daughter noticed a large 2 cm pigmented area on her mother’s wrist, and a biopsy revealed MIS.
NCCN guidelines for MIS recommend surgical excision with margins of 0.5-1 cm but contain a footnote that consideration of topical immunotherapy or radiation therapy is an option in select patients with MIS of the lentigo maligna (LM) subtype, Patel said. He pointed to a retrospective review published 10 years ago looking at 63 MIS/LM cases in which imiquimod 5% cream was used as either primary or adjuvant therapy. When used as primary therapy, with no surgery, 72.7% demonstrated clinical clearance at a mean follow-up of 39.7 (range, 8-95) months.
And when used as adjuvant therapy, 94.4% demonstrated clearance at a mean follow-up of 43.1 (range, 4-106) months. One could opt for primary therapy, knowing that 3 out of 4 patients might have clearance lasting over the course of several-plus years. Or, in the case of adjuvant therapy, “you could do a partial resection or narrow margin resection, and if you have positive margins, go back and have an even higher success rate with adjuvant imiquimod cream,” Patel said.
For his 88-year-old patient, “surgery for a 2 cm tumor on the wrist, with skin that’s fragile, is not easy to accomplish, certainly not easy to close up,” he said. The question was, “could we cause more harm than good?” The patient decided on every-other-day treatment with 5% imiquimod cream for 6 weeks and responded with some clearing. She continued for another 6 weeks but on follow-up was noted to have some areas of progression.
“She ultimately needed an excision as the lesion was progressing in one area, and rebiopsy showed minimal invasion of the MIS, but she was now happy to do so as she felt it was necessary and declared by the disease,” Patel said after the meeting. She was able to undergo an excision with clear margins, and a complex layered closure with a partial skin graft was performed, which she tolerated well.
A Patient With SCC In Situ (SCCis)
Another patient recently referred to Patel for discussion of Mohs surgery was an 89-year-old man who had multiple rough, scaly patches on his bald scalp, a history of prostate cancer, hypertension managed with hydrochlorothiazide, and no family history of melanoma or keratinocyte carcinomas.
Biopsies on two areas of the scalp vertex within 1 cm of each other and one on the neck revealed an SCC in situ on the scalp with an adjacent actinic keratosis (AK). In addition, a biopsy on the neck revealed “AK with focal SCCis,” Patel said at the meeting.
“We’d agree this patient does not need Mohs. But [in this case] we posed a question that was [examined] in a recent study: Does SCC in situ need treatment at all?” Patel said, referring to a single-center cohort study published in 2024 in which 411 consecutive SCCis tumors with a clinically resolved biopsy site were managed with watchful waiting.
Of the 411 tumors, 17 recurred locally (4% recurrence rate), and there were no instances of nodal metastases, distant metastases, or disease-specific death. The highest risk for local recurrence was conferred by a history of solid-organ transplantation (hazard ratio [HR], 9.979; 95% CI, 2.249-39.69), and additional risk factors predicting local recurrence were location of the tumor on the vermillion lip or ear (HR, 9.744; 95% CI, 1.420-69.28) and on the head and neck (HR, 6.687; 95% CI, 1.583-36.15).
The size of the lesion was also predictive of recurrence, with biopsies showing tumor extension to the deep edge being associated with a sixfold increased risk (HR, 6.562; 95% CI, 1.367-39.04). “In typical, run-of-the-mill smaller SCCis, the vast majority of these lesions after biopsy did not recur,” Patel said.
Many experts have proposed the consideration of topical therapy as a first-line treatment for SCCis, but “the question sometimes comes up of whether we can identify patients” at a higher risk for recurrence, he said.
A study published this year of 5-fluorouracil (5-FU) 5% cream for SCCis found that shorter treatment duration (particularly under 2 weeks) and larger lesion size (> 2 cm) were associated with a higher risk for treatment failure. Beyond that, there was no [impact] of immunosuppression or anatomic location, including hair-bearing locations, on the risk of recurrence, Patel said.
The patient decided to pursue 2 weeks of therapy with 5-FU to help mitigate potential side effects, Patel said after the meeting. “He did well….and we decided to monitor after the shortened treatment course.”
Is Intralesional Treatment Coming?
In the future, intralesional treatment may make skin cancer therapy “even easier” for older patients, Patel said at the meeting.
In a case report published in 2024, a 98-year-old wheelchair-bound 80-pound woman with frailty — and a 3.5-cm rapidly growing crusted nodule on her left proximal-lateral arm was treated with intralesional 5-FU — weekly for 4 weeks — after a shave biopsy revealed an invasive, well-differentiated SCC. There was no sign of recurrence at 3 months, and the patient died 6 months later of primary cardiac arrest, Patel said, noting that this was a case “of doing no harm and limiting the morbidity associated with this tumor rather than approaching it from an aggressive standpoint.”
A phase 3 trial of intralesional cemiplimab in patients with early-stage cutaneous SCC, newly underway at GW and multiple other sites, will look at how well the immune checkpoint inhibitor works when injected into the lesion, compared with surgery. The goal is to provide cutting-edge immunotherapy while potentially avoiding systemic toxicity, thus making this a viable nonsurgical option for older patients or those with surgical fatigue, Patel said after the meeting.
Patel disclosed that he had received consulting honoraria from Regeneron Pharmaceuticals, Sun Pharma, Almirall, and Palvella Therapeutics, as well as research support from Regeneron Pharmaceuticals. He had served on the speaker’s bureau with Regeneron Pharmaceuticals, Sun Pharma, and Almirall, and was the cofounder of the Skin Cancer Outcomes Consortium.
Source link : https://www.medscape.com/viewarticle/managing-skin-cancer-older-adults-real-world-cases-2025a1000hdj?src=rss
Author :
Publish date : 2025-06-30 07:09:00
Copyright for syndicated content belongs to the linked Source.