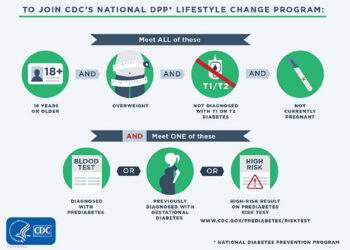
The demand for glucagon-like peptide 1 (GLP-1s) receptor agonists for overweight/obesity has created a clinical conundrum for many primary care providers.
Between 2011 and 2023, obesity-specific prescriptions for GLP-1s increased by 700%. Since then, roughly 1 in 5 Americans have reportedly taken these drugs to lose weight. Given that primary care doctors only have an average of 18 minutes allocated to seeing each patient, how is it possible to conduct routine assessment and comprehensive obesity management?
Though highly effective for weight loss, GLP-1s represent a single piece of the comprehensive management required to not only shed pounds but also prevent weight cycling. This is where lifestyle guidance — nutritional and dietary management coupled with exercise training and behavioral change — becomes essential, and where referrals become a clinical lifeline.
“GLP-1s are tools, not magic pills,” said Clayton F. Runfalo, MD, lead primary care physician at Ochsner Health Center in Gonzales, Louisiana, just outside New Orleans. Runfalo emphasized that he “treats illness but emphasizes wellness.”
“Every patient, every visit I touch on information about healthy choices and healthy living, even if I only spend 30 seconds,” he said.

But practicality is the rule.
“The demands on primary care doctors to see more patients more quickly means that we don’t have time to get into the nuts and bolts. So we frequently refer them out (or in the case of Oschner, to another department) to physicians who understand nutrition and registered dieticians who have the time to spend an hour educating and putting them on a path to succeed,” he said.
A Comprehensive Toolbox
Lifestyle interventions have long been the cornerstone of obesity management, not only to help develop lasting behavioral changes but also to improve overall cardiometabolic outcomes, including dyslipidemia, prediabetes, and hypertension. But many patients are not aware of the impact that GLP-1 agents have on hunger cues, dehydration, and skeletal muscle mass.
“I see a lot of patients who are on different GLP-1s, so I can review nutrition deficits. Are they hydrated; electrolyte balanced? Are they getting enough fiber and still having regular bowel movements?,” said Grace Derocha, MBA, RDN, CDCES, national spokesperson for the Academy of Nutrition and Dietetics.”
“About half of the patients on GLP-1s that I see don’t even know what a protein food is or what a fiber food is,” she said, further reinforcing the need for comprehensive education about avoiding undernutrition while taking these agents.
“I really peel back the layers to get into basic nutrition fundamentals and help build the healthy habit components to address what the patient’s goals are along with how to sustain the improvements in the long run,” said Derocha.
Exercise Beats the Weight Loss Plateau
Maintaining functional muscle mass is also important; data attributed up to 40% of total weight loss to a reduction in lean mass in people taking semaglutide treatment, according to research, increasing risk for frailty, metabolic disturbance, and cardiovascular diseases.

“Sometimes people feel that if the drug is helping them lose weight, they don’t need to do things people normally would do for losing weight, ie, purposeful diet with exercise,” said Evan Matthews, PhD, a cardiologist and exercise physiologist and associate professor, exercise science at Montclair State University in Montclair, New Jersey.
Matthews pointed to additional benefits of initiating an exercise program, especially to counteract the weight loss plateau that inevitably occurs when taking GLP-1s.
“Exercise has been shown to allow patients to reduce their weight further,” he said.
Among 195 patients enrolled in a randomized, placebo-controlled study comparing body fat loss in people who took a GLP-1 and exercised with those who either took the drug but didn’t add exercise or those who exercised but didn’t take the drug, those who followed the combined exercise/drug regimen experienced an additional 3.9 percentage points in lost body fat, which was roughly twice the reduction.
The combination group also saw improvements in the glycated hemoglobin level, insulin sensitivity, and cardiorespiratory fitness.
Matthews said that though more data are needed to guide the combination of the GLP-1s and exercise in terms of “precision” recommendations, “the sooner you start exercise, the sooner you see the benefits. The time it takes to reach a plateau where the patient has to either up the drug or exercise habits will probably be longer,” he said.
“This needs to be thought about as long-term behavior that patients will hopefully do for the rest of their lives. And it will get the patient to a level of fitness that allows them to regain some of the muscle they lost or at least push the body to start maintaining the muscle better,” Matthews said.
Mountains vs Molehills
The need for education, nutritional and dietary changes, building exercise habits, and behavioral changes to sustain changes go part and parcel with GLP-1 treatment. However, Angela Fitch, MD, obesity medicine specialist and chief medical officer and co-founder of Knownwell health clinic in Needham, Massachusetts, near Boston, shared some words of caution.
“A lot of times, we’re making a mountain out of a molehill. The biggest thing to realize is to not make it too onerous,” she said. “You need to have some basic tools at people’s disposal, make sure that they’re eating regularly and not skipping meals because their appetite is suppressed, and focus on whole foods,” said Fitch.

“And if they are not hungry, make sure they are getting protein to supplement. But the point is to simplify and at the very least, hit the basics,” she said. “It’s about having some tools in your toolbox, eg, straightforward handouts or guidance on plants and protein.”
For patients whose insurance coverage is uncertain, Fitch recommended that primary care doctors consider referrals to virtual dietician programs (eg, Nourish or Berry Street) that work with patients to find coverage or offer cash options. Physical therapists (typically covered by insurance) can also fill in the gaps to get exercise routines underway.
The bottom line? “We have to reinforce that these medications are tools. If we don’t have time to spend a half hour or hour teaching them about healthy habits, then by all means, we should be referring them to a dietician, a physical activity specialist or kinesiologist who can dedicate an entire appointment for that,” said Runfalo.
Runfalo, Matthews, and Derocha reported no relevant financial relationships.
Liz Scherer is an independent health and medical journalist.
Source link : https://www.medscape.com/viewarticle/should-you-refer-obesity-patients-comprehensive-weight-2025a10006nt?src=rss
Author :
Publish date : 2025-03-20 10:45:00
Copyright for syndicated content belongs to the linked Source.