Repeated failures in interpreting medical scans have led to delayed cancer diagnoses, unnecessary surgeries, and avoidable deaths, England’s health Ombudsman determined.
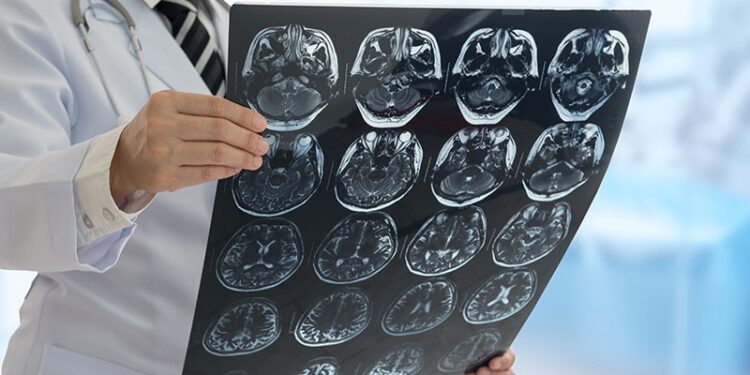
A report by the Parliamentary and Health Service Ombudsman (PHSO) identified recurring issues, including missed abnormalities, delayed or omitted scans, and failures in following up results.
Despite a 2021 report highlighting similar mistakes in the reading and reporting of images, the PHSO said it had since upheld or partly upheld more than 40 cases of related failings.
“Each of the cases we have investigated and upheld represent a real person whose life has been impacted by failings in care,” said Rebecca Hilsenrath KC, PHSO for England.
“In our 2021 report we recommended a system-wide programme of improvements for more effective and timely management of X-rays and scans,” Hilsenrath explained. “While we have seen some progress in this area, unfortunately we are still seeing instances where people’s care is sub-optimal, often with devastating consequences,” she noted in a statement.
Missed Diagnoses
One PHSO investigation found that doctors at Wexham Park Hospital in Slough repeatedly failed to diagnose a man’s cancer. A previous scan had revealed a small bowel lesion, but it was not reported.
The Ombudsman concluded that these failings in care probably contributed to the patient’s decision to end his life. It was recommended that the trust apologise, pay the patient’s daughter £4000, and develop an action plan to prevent future errors.
In another case King’s College London Hospital misidentified a malignant glioblastoma as a benign meningioma, despite repeated scans. The mistakes delayed surgery by 9 months, depriving the patient of timely chemotherapy and radiotherapy.
While glioblastoma has a poor survival rate, the PHSO emphasised that earlier intervention could have extended the patient’s life. The trust was told to apologise, pay £3500, and develop an action plan to prevent reoccurrences.
Other failings included an undiagnosed case of serious pelvic sepsis, which led to an avoidable death, and a missed ankle fracture that resulted in an unnecessary operation.
Severe Radiology Workforce Shortages
A 2023 report by the Royal College of Radiologists (RCR) warned of “dangerous shortages” of doctors essential for diagnosing and treating serious conditions, including cancer and stroke.
The report found that in 2023, 745,290 patients in England waited more than 4 weeks for imaging test results following scans. Workforce shortages were a major factor, with a 30% shortfall in clinical radiology consultants. Without intervention, the college forecast this gap would reach 40% by 2028.
Demand for services is also outpacing consultant growth. While the clinical radiology workforce increased by 6%, demand for computerised tomography (CT) and magnetic resonance imaging (MRI) surged by 11%.
In its State of the wait report, the RCR estimated that an additional 346 radiologists would have been needed in December 2024 to clear the backlog within a month.
Calls for Systemic Change
“The Ombudsman highlights some devastating failures in the NHS, and we must collectively learn from these experiences to drive meaningful change,” commented RCR president Dr Katharine Halliday in a statement.
Hilsenrath stressed that when errors occur, lessons must be learned at both organisational and systemic levels. She called for improvements in NHS digital infrastructure to ensure timely and accurate diagnoses.
“NHS leaders need to address this as the important patient safety issue it is,” she insisted.
Dr Rob Hicks is a retired NHS doctor. A well-known TV and radio broadcaster, he has written three books and has regularly contributed to national newspapers, magazines, and online. He is based in the UK.
Source link : https://www.medscape.com/viewarticle/scan-failures-leading-delayed-diagnoses-and-avoidable-deaths-2025a10006tx?src=rss
Author :
Publish date : 2025-03-21 17:13:00
Copyright for syndicated content belongs to the linked Source.