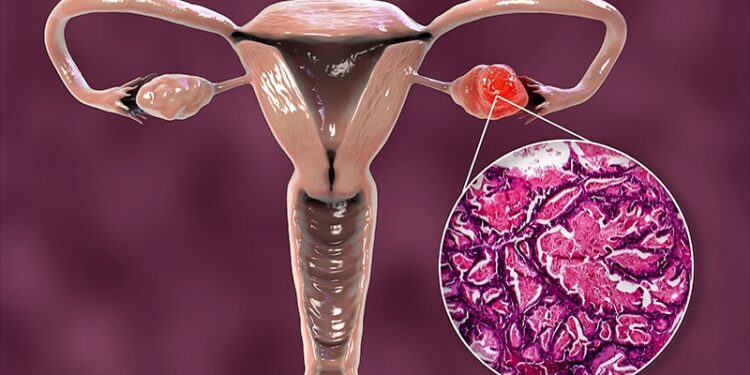
The optimal timing of surgery in patients with resectable advanced ovarian cancer remains controversial. Should these patients receive the standard radical surgery followed by chemotherapy, or could patients do better with chemotherapy before surgery?
The long-awaited TRUST trial aimed to settle this question, but the results paint a somewhat mixed picture.
Among patients with resectable stage IIIB-IVB ovarian cancer, primary cytoreductive surgery followed by chemotherapy led to a statistically significant 2.4-month median progression-free survival (PFS) benefit over neoadjuvant chemotherapy followed by interval cytoreductive surgery. While the median overall survival was 6 months longer in the upfront surgery group, the difference was not statistically significant. Patients in both groups reported similar quality of life over a 3-year period on a global health survey.
“TRUST is the first randomized controlled trial to show a significant benefit in median PFS without compromising short- or long-term quality of life,” said lead investigator Sven Mahner, MD, with Ludwig Maximilian University Hospital, Munich, Germany, who presented the results at the American Society of Clinical Oncology (ASCO) 2025 annual meeting. Mahner called the PFS and overall survival findings in the upfront surgery group “excellent” but acknowledged that the primary endpoint of significant overall survival was not met.
ASCO discussant Emma Barber, MD, gynecologic oncologist with Northwestern Memorial Hospital, Chicago, was less enthusiastic about the benefits of upfront surgery, given the lack of significant overall survival benefit.
Additionally, the upfront surgery group had a higher rate of any complication and more than a twofold higher rate of stoma formation. “There is upfront toxicity with primary debulking surgery compared to neoadjuvant chemotherapy — even in the highest quality surgical centers,” she said.
TRUST Rationale
The aim of surgery in advanced ovarian cancer is to prolong patients’ remission and improve overall survival while sustaining quality of life, said Mahner.
Primary cytoreductive surgery followed by chemotherapy has been considered standard for decades in this patient population. However, there’s an alternative strategy — neoadjuvant chemotherapy followed by interval cytoreductive surgery. Several trials have compared upfront surgery with upfront chemotherapy, but limitations in these studies have not helped answer which approach is better.
TRUST was designed to evaluate the optimal timing of cytoreductive surgery in patients with resectable advanced ovarian cancer who are fit enough to tolerate radical surgery. Patients received care in cancer centers that used defined surgical quality assurance metrics.
Quality criteria were based on the European Training Centre in Gynaecological Oncology certification and included evaluations of cytoreductive surgery in the operating room as well as assessments of surgical proficiency and infrastructure. In addition, participating centers had to have high complete resection rates (at least 50% in upfront surgery for patients with FIGO IIIB-IVB) and high surgical volumes (at least 36 cytoreductive surgeries per year).
Patients were randomly assigned and stratified by center and age-Eastern Cooperative Oncology Group (ECOG) combination (ECOG 0 and age ≤ 65 years vs ECOG > 0 and age older than 65 years) to either primary cytoreductive surgery followed by six cycles of intravenous chemotherapy (n = 345) or three cycles of neoadjuvant chemotherapy followed by interval cytoreductive surgery plus three more cycles of chemotherapy (n = 343).
Most patients had FIGO stage IIIc disease, and over 90% had high-grade serous histology.
Surgical effort was very high in both treatment groups; the median duration of surgery was 5.5 hours in the primary cytoreductive surgery group and 4.5 hours in the interval cytoreductive surgery group, Mahner noted.
High surgical effort led to high complete resection rates — 70% in the primary group and 85% in the interval group — which meant the recommended systemic treatment of carboplatin and paclitaxel could be given in more than 90% of the patients, with a considerable number of patients also receiving bevacizumab or a PARP inhibitor during the course of their disease, Mahner said.
Survival Outcomes
Overall, 219 (64%) PFS events occurred in the primary cytoreductive surgery group and 253 (74%) in the neoadjuvant chemotherapy group. Median PFS after primary surgery was 22.1 months compared to 19.7 months after interval surgery — a 2.4-month benefit (hazard ratio [HR], 0.80; P = .018).
The researchers also conducted a restricted mean survival analysis and found PFS was 31.7 months with primary surgery compared to 26.6 months with neoadjuvant chemotherapy — a 5.1-month benefit (P = .07).
On the overall survival front, the primary surgery group had a 6-month benefit, but the difference was not significant — median overall survival was 54.3 months with primary surgery compared to 48.3 months with interval surgery (HR, 0.89; P = .24).
Careful Patient Selection Necessary
In subgroup analyses, patients with complete cytoreduction after primary surgery had the best outcomes, with a median PFS of 27.9 months vs 21.8 months with interval surgery (HR, 0.69; P = .0009) and median overall survival of 67.0 months vs 55.0 months (HR, 0.80; P = .0521).
In addition, the benefit of primary cytoreductive surgery was most prominent in stage III patients with a median PFS of 26.3 months vs 21.4 months (HR, 0.73; P = .005) and a median overall survival of 63.7 months vs 53.2 months, respectively (HR, 0.84; P = .14). However, patients with stage IV disease did not benefit more from upfront surgery in PFS (HR, 1.01; 95% CI, 0.74-1.38) or overall survival (HR, 0.97; 95% CI, 0.71-1.33).
Mahner also noted that 5 years after randomization, 23% of the patients who had primary surgery had no disease progression compared to 11% of the patients who had interval surgery.
The complication rate was higher in the primary surgery group at 18% vs 12% after interval surgery. The 30-day post-operative mortality rate was less than 1% in both treatment groups. Patients in both groups reported similar quality of life outcomes.
Barber noted that the data suggest that some populations may benefit more from upfront surgery and others may not.
“For example, patients with stage IV disease clearly do not seem to benefit, whereas those with stage III disease seem to show a trend towards improved survival,” she explained.
Given the higher upfront toxicity associated with primary debulking surgery, “selection for primary debulking surgery instead of neoadjuvant chemotherapy should be considered carefully and performed for selected populations,” Barber said.
The study had no commercial funding. Mahner had disclosed relationships with AstraZeneca, Clovis Oncology, GlaxoSmithKline, Janssen-Cilag Ltd., Jenapharm, Medac, Novartis/Pfizer, PharmaMar, Roche/Genentech, Teva Pharmaceuticals, ImmunoGen, Merck, Sensor-Kinesis, Tesaro Inc., Bayer, and Boehringer Ingelheim. Barber had no relevant disclosures.
Source link : https://www.medscape.com/viewarticle/surgery-before-or-after-chemotherapy-advanced-ovarian-cancer-2025a1000fau?src=rss
Author :
Publish date : 2025-06-06 11:09:00
Copyright for syndicated content belongs to the linked Source.