TOPLINE:
Trastuzumab emtansine (T-DM1) demonstrates sustained improvement in invasive disease-free survival and reduced the risk for death in human epidermal growth factor receptor 2 (HER2)-positive breast cancer compared with trastuzumab. At 7 years, invasive disease-free survival and overall survival was 80.8% and 89.1%, respectively, with T-DM1 compared with 67.1% and 84.4%, respectively, with trastuzumab,.
METHODOLOGY:
- Previous analysis of this trial demonstrated that 3-year invasive disease-free survival was significantly higher with T-DM1 compared with trastuzumab (88.3% vs 77.0%; hazard ratio for invasive disease or death, 0.50; P
- The current analysis represents the prespecified final analysis of invasive disease-free survival and second interim analysis of overall survival, providing long-term follow-up data.
- This phase 3, open-label trial randomly assigned 1486 patients HER2-positive breast cancer with residual invasive disease after neoadjuvant therapy to receive either T-DM1 or trastuzumab for 14 cycles.
- Participants received T-DM1 at 3.6 mg per kg intravenously every 3 weeks or trastuzumab at 6 mg per kg intravenously every 3 weeks, with stratification based on clinical stage, hormone-receptor status, preoperative HER2-directed therapy, and pathological nodal status.
- Analysis included a median follow-up of 101.4 months for the T-DM1 group and 100.8 months for the trastuzumab group, with invasive disease-free survival as the primary endpoint and overall survival as a key secondary endpoint.
TAKEAWAY:
- T-DM1 demonstrated superior invasive disease-free survival (hazard ratio [HR], 0.54; 95% CI, 0.44-0.66) and significantly reduced risk for death (HR, 0.66; 95% CI, 0.51-0.87; P = .003).
- Distant recurrence as first invasive-disease event occurred in 14.7% of T-DM1 patients compared with 21.5% in the trastuzumab group, while central nervous system recurrences were documented in 7.0% and 5.1% respectively.
- Adverse events of grade 3 or higher were observed in 26.1% of T-DM1 patients vs 15.7% of trastuzumab patients, with serious adverse events noted in 12.7% and 8.1% respectively.
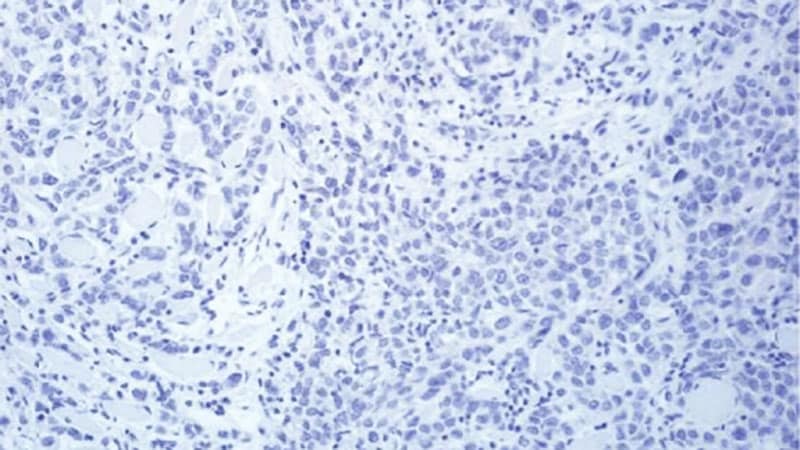
- According to the authors, T-DM1 showed consistent benefit across various subgroups including extent of disease at presentation, hormone-receptor status, and age cohorts, though patients with immunohistochemical (IHC) 2+ disease derived less benefit than the IHC 3+ population.
IN PRACTICE:
“As compared with trastuzumab, T-DM1 improved overall survival with sustained improvement in invasive disease-free survival among patients with HER2-positive early breast cancer with residual invasive disease after neoadjuvant therapy,” wrote the authors of the study.
SOURCE:
The study was led by Charles E. Geyer Jr, MD, NSABP Foundation and University of Pittsburgh School of Medicine-UPMC Hillman Cancer Center in Pittsburgh, Pennsylvania. It was published online on January 16 in The New England Journal of Medicine.
LIMITATIONS:
According to the authors, Black patients were underrepresented in the study population, which may affect the generalizability of the results. The researchers also noted that patients with IHC 2+ and in situ hybridization-amplified disease derived less benefit from T-DM1 compared to the IHC 3+ population, suggesting a need for more effective therapy in this subgroup.
DISCLOSURES:
The study was funded by F. Hoffmann-La Roche/Genentech. The first draft of the manuscript was developed by the first and last authors with assistance from a medical writer paid by the sponsor.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Source link : https://www.medscape.com/viewarticle/trastuzumab-emtansine-ups-long-term-survival-her2-positive-2025a100011u?src=rss
Author :
Publish date : 2025-01-16 12:50:35
Copyright for syndicated content belongs to the linked Source.