The FDA has approved taletrectinib (Ibtrozi, Nuvation Bio) for locally advanced or metastatic ROS1-positive non-small cell lung cancer (NSCLC) in first- and later-line settings, regardless of prior ROS1 tyrosine kinase inhibitor (TKI) exposure.
Taletrectinib is considered a next-generation ROS1 TKI to distinguish it from two first-generation products already on the US market: crizotinib and entrectinib. A third ROS1 TKI approved in 2023, repotrectinib, is also a next-generation medicine.
Like repotrectinib, FDA granted taletrectinib a breakthrough therapy designation.
Compared with crizotinib and entrectinib, Nuvation Bio data suggests taletrectinib has greater brain penetration, lower incidence of neurologic adverse events, less likelihood of resistance, and other benefits, plus a possible safety and efficacy edge over next-generation rival repotrectinib.
“Taletrectinib will likely become the preferred treatment option for advanced ROS1+ NSCLC,” commented Thomas E. Stinchcombe, MD, an associate editor at the Journal of Clinical Oncology, in the “Context” section of his journal’s publication of a pooled analysis of Nuvation Bio’s two approval studies, TRUST-I and TRUST-II, in April.
Taletrectinib was originally developed in China and was approved there in Jan 2025 for the same indication granted by FDA. The company plans a US launch in mid-2025, they stated in a press release.
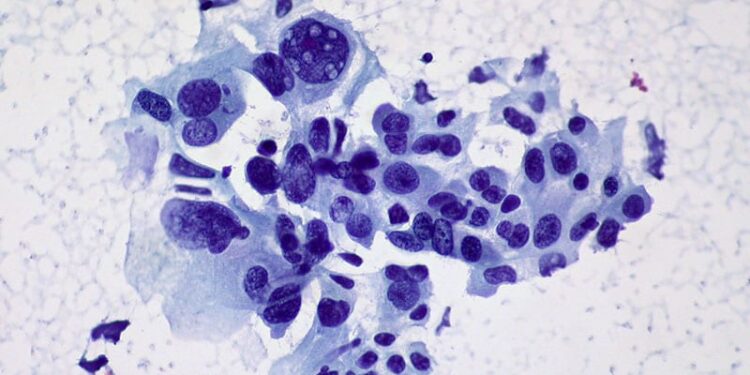
About 2% of NSCLC patients have ROS1-positive disease, and about a third of them present with brain metastases. ROS1-positive patients have an oncogenic rearrangement in the ROS1 gene, which leads to an abnormal ROS1 fusion protein that drives cancer growth. ROS1 TKIs block the protein’s activity.
The drug’s approval was based on results of TRUST-I and TRUST-II, phase 2, single-arm, open label studies in ROS1-positive NSCLC patients treated with oral taletrectinib 600 mg once daily until progression, unacceptable toxicity, death, or consent withdrawal. Of the 273 subjects in the pooled analysis, 93.8% had stage IV disease, 33.7% had brain metastases, and 27.1% had received chemotherapy.
TRUST-I included Chinese subjects who were either new to TKIs or who had received crizotinib. TRUST-II included patients from North America, Europe, and Asia who were TKI-naive or who had been treated with crizotinib or entrectinib.
The efficacy population included 157 patients (103 in TRUST-I; 54 in TRUST-II) who were naive to treatment with a ROS1 TKI and 113 patients (66 in TRUST-I; 47 in TRUST-II) who had received one prior ROS1 TKI. Patients may have received prior chemotherapy for advanced disease.
For treatment-naive patients, the overall response rate (ORR) was 90% in TRUST-I and 85% in TRUST-II, with 72% and 63% of responders having a duration of response (DOR) of at least a year, respectively. For TKI-pretreated patients, ORR was 52% in TRUST-I and 62% in TRUST-II, with 74% and 83% of responders having a DOR of at least 6 months, respectively.
Among 13 patients with a G2032R mutation, which triggers resistance to first generation ROS1 TKIs, eight (61.5%) had a response to taletrectinib.
In a safety analysis with 352 patients, the most frequent treatment-emergent adverse events with taletrectinib were gastrointestinal problems (88%) and elevated aspartate aminotransferase (72%) and alanine aminotransferase (68%). Neurologic adverse events included dizziness (21%) and dysgeusia (15%). Overall, 33% of patients had grade 3 or higher treatment-related adverse events. Treatment-emergent adverse events led to discontinuation in 7% of patients. There were three treatment-related deaths due to abnormal hepatic function, liver failure, and pneumonia.
Prescribing information for taletrectinib includes warnings and precautions for hepatotoxicity, interstitial lung disease/pneumonitis, QTc interval prolongation, hyperuricemia, myalgia with creatine phosphokinase elevation, skeletal fractures, and embryo-fetal toxicity.
The recommended taletrectinib dose is 600 mg orally once daily on an empty stomach until disease progression or unacceptable toxicity.
Taletrectinib pricing was not available, but fourteen 160 mg capsules of rival repotrectinib — the initial 2-week supply with daily dosages doubling afterwards — is $7,666.97, according to drugs.com.
M. Alexander Otto is a physician assistant with a master’s degree in medical science and a journalism degree from Newhouse. He is an award-winning medical journalist who worked for several major news outlets before joining Medscape. Alex is also an MIT Knight Science Journalism fellow. Email: [email protected]
Source link : https://www.medscape.com/viewarticle/taletrectinib-approved-nsclc-2025a1000fpx?src=rss
Author :
Publish date : 2025-06-11 20:57:00
Copyright for syndicated content belongs to the linked Source.